|
Clinical Practice Guidelines - Third Edition
NOTE: August 6, 2006
The latest update of the Guidelines can be found at:
http://www.rsdfoundation.org/en/en_clinical_practice_guidelines.html
Printer Friendly Version
Reflex Sympathetic Dystrophy / Complex Regional Pain Syndrome (RSD/CRPS)
Anthony F. Kirkpatrick, M.D., Ph.D.
Editor
Department of Anesthesiology
University of South Florida
Tampa, Florida
International Research Foundation for RSD/CRPS
Last update: January 1, 2003
Preface to the Third Edition
The first "International Update on RSD/CRPS" was held at the University of South Florida on February 1 and 2, 2002. Thanks to the organizational efforts of Dr. Srinivasa Raja at John Hopkins University, the symposium presented
an outstanding faculty of international experts on RSD/CRPS. The symposium formed a foundation for writing the third edition of the Clinical Practice Guidelines.
The Clinical Practice Guidelines have become
a standard for managing RSD/CRPS. As with prior editions, my intention has been to focus on providing health care providers and patients unbiased information that will enable patients to make informed choices about
their treatment. As noted in a recent issue of the JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION, the information had to be carefully selected and organized. * One of the major reasons why physicians do not follow
clinical practice guidelines is that most are not concise enough for both physicians and patients to read, understand and follow. Guidelines need to be presented in a concise manner saying in effect, "These measures
are recognized as essential, these others should be considered, and this group has been found ineffective or contraindicated."
The most notable addition to third edition is a new section titled "RSD in Children."
During the course of preparing this section, it was necessary to consult extensively with experts in the field of pediatric pain management. These persons included Dr. Sabine Kost-Byerly at Johns Hopkins University,
Dr. Robert Wilder at Mayo Clinic and Dr. Robert Schwartzman at Allegheny University of Health Sciences. Their efforts were a significant factor in completing the third edition, for which I am most appreciative.
The Scientific Advisory Committee has reviewed and commented on the third edition of the Guidelines. These persons were chosen because of their acknowledged expertise worldwide in the area of RSD/CRPS. The members of
the Committee are listed on the Foundation's web site. If you would like to see a list of the Committee members, please click here.
Last, but not least, I am grateful to the patients
and health providers throughout the world who took the time to provide feedback on the second edition. The Foundation welcomes feedback on the clinical practice guidelines at "Contact Us".
Anthony F. Kirkpatrick, M.D., Ph.D.
Chair, Scientific Advisory Committee
Director of Research
January 1, 2003
* Veatch RM, Montgomery AA, Dahlberg, K, Cabana MD, Rand CS, Powe NR, Wu AW, Abboud PC, Wilson MH. Reasons physicians do not follow clinical practice guidelines. JAMA 2000; 283: 1685-1686.
Contents:
Diagnosis
Treatment
Photo Gallery
Opioid Treatment Protocol
External Battery System Vs Internal Battery System
How to Determine the Effectiveness of Treatments
RSD In Children --- NEW!
References
Glossary of Medical Terms
REFLEX SYMPATHETIC DYSTROPHY SYNDROME
(RSD/CRPS)
Reflex Sympathetic Dystrophy Syndrome (RSD) is also known as Complex Regional Pain Syndrome (CRPS). RSD/CRPS is a multi-symptom, multi-system, syndrome usually affecting one or more extremities, but may affect virtually
any part of the body. Although it was clearly described 125 years ago by Drs. Mitchell, Moorehouse and Keen, RSD/CRPS remains poorly understood and is often unrecognized.
The best way to describe RSD/CRPS is
in terms of an injury to a nerve or soft tissue (e.g. broken bone) that does not follow the normal healing path. The development of RSD/CRPS does not appear to depend on the magnitude of the injury (e.g. a sliver in
the finger can trigger the disease). In fact, the injury may be so slight that the patient may not recall ever having received an injury. For reasons we do not understand, the sympathetic nervous system seems to assume
an abnormal function after an injury. There is no single laboratory test to diagnose RSD/CRPS. Therefore, the physician must assess and document both subjective complaints (medical history) and, if present, objective
findings (physical examination), in order to support the diagnosis. There is a natural tendency to rush to the diagnosis of RSD/CRPS with minimal objective findings because early diagnosis is critical. If undiagnosed
and untreated, RSD/CRPS can spread to all extremities, making the rehabilitation process a much more difficult one. If diagnosed early, physicians can use mobilization of the affected extremity (physical therapy) and
sympathetic nerve blocks to cure or mitigate the disease. If untreated, RSD/CRPS can become extremely expensive due to permanent deformities and chronic pain. There are no studies showing that RSD/CRPS affects the patient's
life span. The potential exists for long-term financial consequences. At an advanced state of the illness, patients may have significant psychosocial and psychiatric problems, they may have dependency on narcotics and
may be completely incapacitated by the disease. The treatment of patients with advanced RSD is a challenging and time-consuming task.
Diagnosis
If one can demonstrate major nerve damage associated with the development of RSD/CRPS symptoms, the condition is called complex regional pain syndrome (CRPS) type II or causalgia. Generally, causalgia provides more objective
evidence of disease due to neurological changes (numbness and weakness).
The terms complex regional pain syndrome (CRPS) type I and type II have been used since 1995, when the International Association for
the Study of Pain (IASP) felt the respective names reflex sympathetic dystrophy and causalgia were inadequate to represent the full spectrum of signs and symptoms. 1-8 The term "Complex" was added to convey the reality that RSD and causalgia express varied signs and symptoms. Many publications, particularly older ones, still use the names RSD and causalgia. To facilitate
communication and understanding the designation RSD/CRPS is generally used throughout these practice guidelines. The principles applicable to the diagnosis and management of RSD are similar to those principles applicable
to the diagnosis and management of causalgia.
To make the early diagnosis of RSD/CRPS, the practitioner must recognize that some features/manifestations of RSD/CRPS are more characteristic of the syndrome than
others, and that the clinical diagnosis is established by piecing each bit of the puzzle together until a clear picture of the disorder emerges. Often the physician needs to rule out other potentially life-threatening
disorders that may have clinical features similar to RSD/CRPS, e.g. a blood clot in a leg vein or a breast tumor spreading to lymph glands can cause a swollen, painful extremity. Indeed, RSD/CRPS may be a component
part of another disease, (e.g. a herniated disc of the spine, carpal tunnel syndrome of the hand, heart attack). Thus, treating RSD/CRPS will often be directed to treating clinical features rather than a well defined
disease. When RSD/CRPS spreads the diagnosis can be more complicated. For example, if it spreads to the opposite limb, it may be more difficult to establish a diagnosis because there is no normal side (control) to compare
for objective findings. On the other hand, the spreading of RSD/CRPS symptoms may actually facilitate the diagnosis of RSD/CRPS because spreading symptoms is a characteristic of the disorder. (See below).
Importance of Objective Findings
Many patients who develop RSD/CRPS as the result of an injury do so in the context of legal liability. Some patients can be expected to defend their rights in courts of law. It is not uncommon for the defendant to accuse
the patient of faking their condition, especially if there are no objective findings for RSD/CRPS documented on the medical record. Therefore, the evaluating physician must assess more than just subjective complaints
(medical history). The physician must
aggressively seek and document objective findings. For example, about 80% of RSD/CRPS cases have differences in temperature in opposite sides that may be either colder or warmer. These temperature changes may
be associated with changes in skin color. Furthermore, the temperature differences are not static. The skin temperature can undergo dynamic changes in a relatively short period of time (within minutes) depending critically
on room temperature, local temperature of the skin and emotional stress. In some cases, the differences in temperatures may fluctuate spontaneously even without any apparent provocation. 4 Thus, the objective finding of differences in temperature and color of the skin can be missed by the physician if only a single physical examination is made. A useful and relatively inexpensive instrument to have available
at the time of the physical examination is a portable infrared thermometer to measure differences in skin temperature. Changes in skin temperature and color are only two examples of several objective findings that should
be sought in the patients with RSD/CRPS.
Making the Diagnosis of RSD/CRPS
The diagnosis of RSD/CRPS can be made in the following context. A history of trauma to the affected area associated with pain that is disproportionate to the inciting event plus one or more of the following:
- Abnormal function of the sympathetic nervous system.
- Swelling.
- Movement disorder.
- Changes in tissue growth (dystrophy and atrophy).
Thus patients do not have to meet all of the clinical manifestations listed above to make the diagnosis of RSD/CRPS. The new CRPS classification system acknowledges this fact by stating that some patients with RSD/CRPS
may have a third type of CRPS by categorizing it as
"otherwise not specified". There seems to be a small group of patients whose pain following trauma resolves over time, leaving the patient with a movement disorder. The pain and symptoms of RSD/CRPS
may exceed both the magnitude and duration of symptoms expected from the normal healing process expected from the inciting event. Similarly, the RSD/CRPS diagnosis is precluded by the existence of known pathology that
can be explained by the observed symptoms and degree of pain. There are "grades" of this syndrome described in the literature with symptoms ranging from minor to severe.
Clinical Features of RSD/CRPS
-
Pain - The hallmark of RSD/CRPS is pain and mobility problems out of proportion to those expected from the initial injury. The first and primary complaint occurring in one or more extremities is
described as severe, constant, burning and/or deep aching pain. All tactile stimulation of the skin (e.g. wearing clothing, a light breeze) may be perceived as painful (allodynia). Repetitive tactile stimulation
(e.g. tapping on the skin) may cause increasing pain with each tap and when the repetitive stimulation stops, there may be a prolonged after-sensation of pain (hyperpathia). There may be diffuse tenderness or
point-tender spots in the muscles of the affected region due to small muscle spasms called muscle trigger points (myofascial pain syndrome). There may be spontaneous sharp jabs of pain in the affected region
that seem to come from nowhere (paroxysmal dysesthesias and lancinating pains).
-
Skin changes - skin may appear shiny (dystrophy-atrophy), dry or scaly. Hair may initially grow coarse and then thin. Nails in the affected extremity may be more brittle, grow faster and then
slower. Faster growing nails is almost proof that the patient has RSD/CRPS. RSD/CRPS is associated with a variety of skin disorders including rashes, ulcers and pustules. 9 Although extremely rare, some patients have required amputation of an extremity due to life-threatening reoccurring infections of the skin. Abnormal sympathetic (vasomotor changes) activity may be associated
with skin that is either warm or cold to touch. The patient may perceive sensations of warmth or coolness in the affected limb without even touching it (vasomotor changes). The skin may show increased sweating
(sudomotor changes) or increased chilling of the skin with goose flesh (pilomotor changes). Changes in skin color can range from a white mottled appearance to a red or blue appearance. Changes in skin color
(and pain) can be triggered by changes in the room temperature, especially cold environments. However, many of these changes occur without any apparent provocation. Patients describe their disease as though
it had a mind of its own.
-
Swelling - pitting or hard (brawny) edema is usually diffuse and localized to the painful and tender region. If the edema is sharply demarcated on the surface of the skin along a line,
it is almost proof that the patient has RSD/CRPS. However, some patients will show a sharply demarcated edema because they tie a band around the extremity for comfort. Therefore, one has to be certain
that the sharply demarcated edema is not due to a previously wrapped bandage around the extremity.
-
Movement Disorder - Patients with RSD/CRPS have difficulty moving because they hurt when they move. In addition, there seems to be a direct inhibitory effect of RSD/CRPS on muscle contraction.
Patients describe difficulty in initiating movement, as though they have "stiff" joints. This phenomena of stiffness is most noticeable to some patients after a sympathetic nerve block
when the stiffness may disappear. Decreased mobilization of extremities can lead to wasting of muscles (disuse atrophy). Some patients have little pain due to RSD/CRPS but instead they have a great
deal of stiffness and difficulty initiating movement.7 Tremors and involuntary severe jerking of extremities may be present. Psychological stress may
exacerbate these symptoms. Sudden onset of muscle cramps (spasms) can be severe and completely incapacitating. Some patients describe a slow "drawing up of muscles" in the extremity due
to increased muscle tone leaving the hand-fingers or foot-toes in a fixed position (dystonia). Patients with such seemly bizarre movements might be inaccurately diagnosed with a psychogenic movement
disorder. Additionally, the fact that quite extreme behavioral changes often follow rather trivial injuries in patients with RSD/CRPS, this observation might contribute to the perception that the
patient suffers from a psychogenic disorder as well.
Specific diagnostic criteria have been established for the diagnosis of psychogenic movement disorders in cases involving RSD/CRPS.
10 Unfortunately, physicians sometimes fail to follow these diagnostic guidelines and carelessly report a "psychogenic" disorder. 11 This misdiagnosis can be devastating to the patient and can lead to delaying urgent medical care.
A clinical test sometimes used to demonstrate that a patient is faking muscle weakness is
called "give away weakness". This test is NOT a reliable indicator of a psychogenic movement disorder. Patients with RSD/CRPS will give away when a force is applied to their extremity because of
pain. Also, because patients with RSD/CRPS have difficulty sustaining muscle contraction, they will give away as well.
- Spreading Symptoms
- Initially, RSD/CRPS symptoms are generally localized to the site of injury. As time progresses, the pain and symptoms tend to become more diffuse. Typically, the disorder starts in an extremity.
However, the pain may occur in the trunk or side of the face. On the other hand, the disorder may start in the distal extremity and spread to the trunk and face. At this stage of the disorder,
an entire quadrant of the body may be involved. Maleki et. al. recently described three patterns of spreading symptoms in RSD/CRPS: 12
-
A "continuity type" of spread where the symptoms spread upward from the initial site, e.g. from the hand to the shoulder.
-
A "mirror-image type" where the spread was to the opposite limb.
-
An "independent type" where symptoms spread to a separate, distant region of the body. This type of spread may be related to a second trauma.
-
Bone changes - X-rays may show wasting of bone (patchy osteoporosis) or a bone scan may show increased or decreased uptake of a certain radioactive substance (technecium 99m)
in bones after intravenous injection.
-
Duration of RSD/CRPS - The duration of RSD/CRPS varies, in mild cases it may last for weeks followed by remission; in many cases the pain continues for years and in some
cases, indefinitely. Some patients experience periods of remission and exacerbation. Periods of remission may last for weeks, months, or years.
Stages of RSD/CRPS:
The staging of RSD/CRPS is a concept that is dying. The course of the disease seems to be so unpredictable between various patients that staging is not helpful in the treatment of RSD/CRPS. Not all of the clinical features
listed below for the various stages of RSD/CRPS may be present. The speed of progression varies greatly in different individuals. Stage I and II symptoms begin to appear within a year. Some patients do not progress
to Stage III. Furthermore, some of the early symptoms (Stage I and II) may fade as the disease progresses to Stage III. The following stages are presented in these guidelines merely for historical significance.
STAGE I
-
Onset of severe, pain limited to the site of injury
-
Increased sensitivity of skin to touch and light pressure (hyperasthesia).
-
Localized swelling
-
Muscle cramps
-
Stiffness and limited mobility
-
At onset, skin is usually warm, red and dry and then it may change to a blue (cyanotic) in appearance and become cold and sweaty.
-
Increased sweating (hyperhydrosis).
-
In mild cases this stage lasts a few weeks, then subsides spontaneously or responds rapidly to treatment.
STAGE II
-
Pain becomes even more severe and more diffuse
-
Swelling tends to spread and it may change from a soft to hard (brawny) type
-
Hair may become coarse then scant, nails may grow faster then grow slower and become brittle, cracked and heavily grooved
-
Spotty wasting of bone (osteoporosis) occurs early but may become severe and diffuse
-
Muscle wasting begins
STAGE III
-
Marked wasting of tissue (atrophic) eventually become irreversible.
-
For many patients the pain becomes intractable and may involve the entire limb.
-
A small percentage of patients have developed generalized RSD affecting the entire body. 6
Photo Gallery
Dr. Robert J. Schwartzman, whose name is synonymous with RSD/CRPS, has contributed a photo gallery to the Clinical Practice Guidelines. His photos illustrate some of the objective findings that may be observed in patients
with RSD/CRPS. It should be emphasized that patients with RSD/CRPS may not present with these objective findings, especially during the early stages of the disease.
Dr. Schwartzman is Professor and Chairman of the Department of Neurology at Hahnemann School of Medicine in Philadelphia, PA, USA. He is a member the Scientific Advisory Committee. Through his numerous publications,
lectures, and research efforts, he shares his clinical experience by making others aware of the effects of RSD/CRPS. Dr. Schwartzman has received several honors and awards, including the Mayo Clinic Neurology Teaching
Award and the Dean's Special Award for Excellence in Teaching from Hahnemann University of Medicine in both 1998 and 1999.
Pictures 1 - 4
Pictures 5 - 8
Pictures 9 - 12
Pictures 13 -16
Some other names given to this syndrome:
-
Causalgia (Minor or Major)
-
Sudeck's Atrophy
-
Post Traumatic Dystrophy (Minor or Major)
-
Shoulder Hand Syndrome
-
Reflex Neurovascular Dystrophy
Incidence of RSD/CRPS:
-
The exact prevalence of RSD/CRPS is unknown; however, data from several studies suggest it is more frequent than commonly believed.
-
Both sexes are affected, but the incidence of the syndrome is higher in women, especially in the pediatric population.
Etiology:
-
A number of precipitating factors have been associated with RSD/CRPS including:
-
Trauma (often minor) ranks as the leading provocative event
-
Ischemic heart disease and myocardial infarction
-
Cervical spine or spinal cord disorders
-
Cerebral lesions
-
Infections
-
Surgery
-
Repetitive motion disorder or cumulative trauma, causing conditions such as carpal tunnel.
However, in some patients a definite precipitating event can not be identified.
Cause of RSD/CRPS
Current research suggest that the mechanism by which an injury triggers RSD/CRPS is unclear. Figure 1 is intended to give the reader a simplified view of how an injury might lead to the symptoms of RSD/CRPS.
Figure 1
Activation of the sympathetic nervous system following an injury is part of a fright-flight response to an emergency situation. This response is very important for survival. For example, firing of sympathetic nerves causes
blood vessels in the skin to contract, forcing blood deep into muscle and enabling the victim to use his muscle to get up after an acute injury and escape from further danger. Also the decreased supply of blood to the
skin reduces blood loss through superficial injuries that may occur on the surface of the body. Ordinarily, the sympathetic nervous system shuts down within minutes to hours after an injury. For reasons we do not understand,
individuals who go on to develop RSD/CRPS, the sympathetic nervous system appears to assume an abnormal function. Theoretically, this sympathetic activity at the site of injury could cause an inflammatory response causing
the blood vessels to spasm leading to more swelling and pain. (See B, C, and D in Figure 1) The events could lead to more pain which triggers another response, establishing a vicious cycle of pain.
For a video animation depicting how an injury might trigger RSD/CRPS:
CLICK HERE
Failure to mobilize the affected region of the body might be a critical factor in prolonging the recovery from RSD/CRPS. However, disuse of muscle does not appear to be responsible for the genesis of RSD/CRPS. For example,
investigators in Sweden have reported highly unusual data that makes it difficult to explain the genesis of RSD/CRPS simply on the basis of disuse. They carried out a pathological analysis of peripheral nerve and muscle
taken from amputated legs of eight patients with RSD/CRPS. 13 In all patients, amputation was performed because the painful (hyperpathic) limb was useless or subject to
recurrent infections. Skeletal muscle specimens were abnormal in all cases, but myelinated nerve fibers were normal, and in half the patients there was a loss of unmyelinated fibers. These findings suggest a microangiopathy
in the affected limbs. Thus, patients with RSD/CRPS have tissues that are truly abnormal, and abnormal in ways that cannot be readily explained by disuse and/or psychological factors.
Laboratory Diagnostic Aids:
There is no laboratory test that can stand alone as proof of RSD/CRPS. However, there are a couple of tests (thermogram and bone scan) which can be useful in providing evidence for RSD/CRPS.
Thermogram - A thermogram is a noninvasive means of measuring heat emission from the body surface using a special infrared video camera. It is one of the most widely used tests in
suspected cases of RSD/CRPS. As noted, detecting an abnormal change in skin temperature in RSD/CRPS depends on many factors. A normal thermogram does not necessarily mean the patient does not have RSD/CRPS. An abnormal
thermogram may be helpful when there are minimal objective findings for RSD/CRPS documented in the medical record. Furthermore, certain patterns of abnormal heat emission from the body (e.g. circumferential versus
dermatomal changes) are more indicative of the existence of RSD/CRPS than others. The thermogram should be performed at a reputable medical facility. The quality of the test may vary among providers.
Three phase radionuclide bone scanning - the role of the 3 phase bone scan in the diagnosis of RSD/CRPS has been debated and is controversial.
Sympathetic blocks - See below under "sympathetic blocks".
X-rays, EMG, Nerve Conduction Studies, CAT scan and MRI studies - All of these tests may be normal in RSD/CRPS. These studies may help to identify other possible causes
of pain; for example, RSD/CRPS plus a carpal tunnel syndrome.
Treatment
The single most important modality for treating the patient with RSD/CRPS is education. The informed consent process should be the focus of education. The physician defines the potential benefits, risks, alternatives (and
costs). From the start, the therapeutic goals must be defined and accepted by the patient:
-
Educate About Therapeutic Goals
-
Encourage Normal Use of the Limb (Physical Therapy)
-
Minimize Pain
-
Determine the Contribution of the Sympathetic Nervous System to the Patient's Pain
The cornerstone in the treatment of RSD/CRPS is normal use of the affected part as much as possible. Therefore, all modalities of therapy (drugs, nerve blocks, TENS, physical therapy, etc.) are employed to facilitate movement
of the affected region of the body. Although physical therapy is an important treatment modality, significant misuse and overuse of this modality may occur. Often the physical therapist will treat the patient with RSD/CRPS
the same as a stroke or a nerve plexus injury, (which will fail due to extreme pain and possible injury with passive manipulation). The primary goal of the physical therapist should be to teach the patient how to use
their affected body part through activities of daily living. Swimming pool exercises are very helpful, especially for RSD/CRPS of the lower extremity where weight-bearing can be problematic. The goal of physical therapy
should be to create independence from the health care system in the shortest period. Learning that "to hurt is not to harm" is difficult, but it is essential to avoid reinjury.
Learning the non-protective
nature of pain due to RSD/CRPS takes time. For patients who are significantly impaired in their ability to mobilize their extremity, it is urgent to offer the patient the opportunity to determine the contribution of
their sympathetic nervous system to their pain. This is accomplished by a sympathetic nerve block to the affected extremity (Figure 2). Future therapeutic options for the patient will depend on whether their pain is
determined to be sympathetically maintained pain (SMP) or sympathetically independent pain (SIP). Published reports suggest that the best response to sympathetic blocks will occur if the blocks are given as soon as
possible during the course of the disease.
The "LET'S TRY THIS NOW" approach is to be deplored because it indicates that the physician has not defined a strategy to achieve specific therapeutic goals
in the shortest period of time. It also adds to the confusion, frustration, anxiety and depression of the patient, which may intensify the patient's pain and adversely effect the doctor-patient relationship.
Figure 2
1. Establish a written treatment protocol.
Figure 2 illustrates a typical treatment protocol that was designed to rehabilitate the patient in the shortest possible time. Initiate the safest, simplest, and most cost-effective therapies first. If the patient fails
to progress in mobilizing the extremity, it is essential to offer the patient a series of 3 sympathetic blocks immediately. The purpose of the sympathetic blocks is three-fold: to treat, to diagnose if the pain is sympathetically
maintained and to provide prognostic information. The sympathetic block provides a prognostic indicator if sympathectomy or other treatment modalities would be the next appropriate step. Sympathetic blocks are discussed
in detail below.
After the physician has completed a defined course of treatment (e.g. a series of 3-6 sympathetic blocks), it would be helpful to prepare an update report that would document the patient's
response to the course of treatment. The report should reflect a basis for further treatment and it should address future rehabilitation needs. Sharing a copy of the update report with the patient will help ensure that
all parties are kept informed. Sharing the report with the patient helps keep the patient and physician focused on achieving appropriate therapeutic goals. An update report should address five areas of care:
-
Procedures (e.g. nerve blocks)
-
Medications
-
Physical/occupational therapy
-
Psychosocial issues
-
New laboratory tests or consults
2. Psychosocial modalities must be considered in all patients with RSD/CRPS.
Psychiatric illness or personality disorder does not cause RSD/CRPS but it is likely that personality contributes to the disease. 14,15 Patients with severe, advanced stage
RSD/CRPS usually undergo a psychosocial evaluation during the series of sympathetic blocks or prior to offering the patient more invasive treatments. In some cases, a formal psychosocial evaluation should be initiated
much earlier in the course of treatment. For example, children with RSD/CRPS may require a thorough evaluation to determine the family support structure and the coping mechanisms needed by the family for optimal rehabilitation
of the child.
For a free 4-minute video on the emotional consequences of RSD/CRPS in children:
CLICK HERE
The psychosocial evaluation should always be done by an expert in chronic pain and should always include an assessment of pain coping skills and drug abuse potential. Stress is a known cause of exacerbation of this disease,
making emergency treatment more necessary. A lot of memorials sent to fund RSD/CRPS research are the result of suicides!
The potential for committing suicide needs to be assessed. The patient may need to participate in a formal pain management program as an outpatient or an inpatient. Chronic pain patients referred
for a psychosocial evaluation tend to be defensive. An MMPI or other psychological test can help identify the psychosocial problems. Patients must be properly motivated to improve their coping skills; otherwise, application
of these psychosocial modalities is a waste of time. Relaxation techniques (e.g. breathing exercises) as well as biofeedback and self-hypnosis may be appropriate treatment modalities for some patients.
3. Sequential Drug Trials:
Try to initiate sequential trials for each modality of therapy. The application of multiple therapies at the same time, a shotgun approach, makes it almost impossible to evaluate and optimize an individual therapy for safety
and efficacy. Patients must be advised that the optimal dose for medications varies greatly among patients. Therefore, it is usually necessary to gradually increase the dose of their medication to the point of significant
toxicity in order to determine optimal dose. The dose is then reduced to the next lower level. Thus it is important for the patient to become familiar with all of the potential side effects of a medication before trying
it. Sequential trials with many different drugs may be required to determine the best medication for the patient.
Medications are generally prescribed according to the following characteristics of the pain:
-
Constant pain
-
Pain causing sleep problems
-
Inflammatory pain or pain due to recent tissue injury
-
Spontaneous jabs (paroxysmal dysesthesias and lancinating pain)
-
Sympathetically maintained pain (SMP)
-
Muscle cramps
Medications used to treat chronic pain:
"Off-labeling" prescribing means that a government (e.g., the U.S. Food and Drug Administration - FDA) approved the medication for one purpose but it is used by physicians for another purpose. For example, aspirin
is a pain medication but it can also be used to decrease the risk of a heart attack by inhibiting the aggregation of platelets. Off-label prescribing is a common practice in treating various chronic pain problems. Some
of these drugs have been proven to be effective in decreasing pain due to nerve injury (neuropathic pain) in well-controlled clinical trials. Since RSD/CRPS is believed to be caused by nerve injury (neuropathic pain),
these drugs are used to treat this condition as well. The patient should consider weaning themselves from these various medications periodically with the treating physician's knowledge to determine for themselves that
the medication is actually helping to alleviate their symptoms. Some medications need to be weaned slowly (e.g. narcotics, baclofen) to minimize withdrawal symptoms.
Medications commonly used to treat RSD/CRPS based on the type of pain include:
For constant pain associated with inflammation:
Nonsteroidal anti-inflammatory agents (e.g. aspirin, ibuprofen, naproxen, indomethacin, etc).
For constant pain not caused by inflammation:
Agents acting on the central nervous system by an atypical mechanism (e.g. tramadol)
For constant pain or spontaneous (paroxysmal) jabs and sleep disturbances;
Anti-depressants (e.g. amitriptyline, doxepin, nortriptyline, trazodone, etc) 1,6
Oral lidocaine (mexilitine - some what experimental)
For spontaneous (paroxysmal) jabs
Anti-convulsants (e.g. carbamazepine, gabapentin may relieve constant pain as well) 17-19
For widespread, severe RSD/CRPS pain, refractory to less aggressive therapies
Oral opioid. The use of opioids (e.g. narcotics with names such as Darvon, Vicodin, Loratab, Percocet, morphine, codeine, etc) to treat RSD/CRPS is debated and there are potential hazards.
Therefore, in order to ensure appropriate informed consent, it is recommended that the patient sign a doctor-patient "contract." A typical doctor-patient contract can be found by clicking on the link below.
20
CLICK HERE FOR OPIOID TREATMENT PROTOCOL
Patients may require immediate and adequate pain relief. In some cases it may take time to transpire from the time of the patients first visit to the time of adequate treatment. In all probability, the pain and degenerative
cycle would progress. Since the abuse potential is minimal when narcotics are used for severe pain, practitioners should not withhold narcotic treatment, if the patient demonstrates pain relief with this medication.
For the treatment of sympathetically maintained pain (SMP)
Clonidine Patch. Studies suggest that clonidine may decrease pain in RSD/CRPS by inhibiting the sympathetic nervous system. 21,22 A treatment protocol for using the
Clonidine Patch to treat RSD/CRPS can be found in the journal Regional Anesthesia. 23
For muscle cramps (spasms and dystonia) which can be very difficult to treat.
Klonopin (clonazepam)
Baclofen
For localized pain related to nerve injury.
Capsaicin cream. (This medication is applied to the skin and behaves like hot peppers. The effectiveness of capsaicin cream in the treatment of RSD/CRPS has not been determined). 24
4. Physical and Occupational Therapy:
Patients need to be educated on how to use their affected body part through activities of daily living. For example, for lower extremity RSD/CRPS, patients may need to be taught weight bearing versus non-weight bearing
exercises. Hydrotherapy is usually medically necessary for muscle (myofascial) pain and spasms. Application of pressure (massage) and/or moist heat applications can sometimes relieve severe muscle cramps. The physical
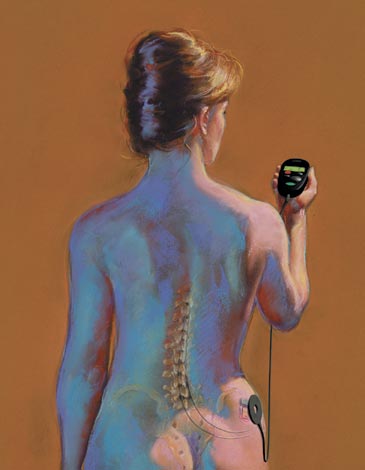
therapist can also teach the patient how to use a TENS unit (a noninvasive electrical device that stimulates the surface of the skin). Pool therapy can be very effective for improving mobility.
5. Sympathetic Blocks:
There are three reasons to consider sympathetic blockade to facilitate the management of RSD/CRPS. First, the sympathetic block may provide a permanent cure or partial remission of RSD/CRPS. Second, by selectively blocking
the sympathetic nervous system the patient (and physician) will gain further diagnostic information about what is causing the pain. The sympathetic block helps determine what portion of the patient's pain is being
caused by malfunction of their sympathetic nervous system. Third, the patient's response to a sympathetic block provides prognostic information about the potential merits of other treatments. 25-27
There is evidence that there might be a role for sympathetic blocks in preventing RSD/CRPS. A retrospective study demonstrated that the prophylactic use of sympathetic blocks in patients with a history
of RSD/CRPS decreased the occurrence rate of the disease from 72% to 10% after re-operation on the affected extremity. 28
If sympathetic blocks are not properly
performed and evaluated, time and money will be wasted, and diagnostic-prognostic information will be lost. A good sympathetic block should increase the temperature of the extremity without producing increased numbness
or weakness. The sensation of warmth tells the patient that they have had a sympathetic block. If the block causes numbness or weakness, more than just the sympathetic nerves were blocked and the patient will get
an overestimation of the amount of their pain that is contributed by their sympathetic nervous system; hence, the diagnostic and prognostic value of the nerve block would be lost. The amount of pain relief and improvement
in range of motion and in exercise tolerance should be noted by the patient and recorded by the physician. This information about the patient's response to sympathetic blockade will serve as a prognostic indicator
for rehabilitation following the series of sympathetic blocks and it will help the patient decide if a permanent block (destruction of the nerve by sympathectomy) would be appropriate. Also, the information will
aid in directing future medications in a more rational manner. Some patients will experience a "booster effect" with each sympathetic block, i.e. each successive sympathetic block in the series provides
greater and greater pain relief and improvement in exercise tolerance. The maximum sustained benefit from a series of sympathetic blocks is usually apparent after a series of 3-6 blocks. Even if the original site
is unresponsive to sympathetic blockade, future exacerbation of RSD/CRPS symptoms at the same site or at a distant site may be responsive to 1-3 sympathetic blocks. THE GOAL IS ALWAYS TO TREAT BUT DON'T OVER TREAT.
Sympathetic blocks are usually performed by a pain specialist trained in anesthesia. In experienced hands, these nerve blocks can be performed with minimal discomfort to the patient with or without IV
sedation. Complications from sympathetic blockade are extremely rare. However, it is always possible for the local anesthetic to be inadvertently injected into a blood vessel or into the spinal fluid. If this should
happen, the patient may temporarily become weak and lose consciousness. For safety reasons, sympathetic blocks are always performed under conditions where the vital signs (blood pressure and breathing) can be monitored
closely. Patients should not eat for 6 hours prior to a sympathetic block. For further information about safety in performing nerve blocks refer to the web site for the Anesthesia Patient Safety Foundation: http://gasnet.med.yale.edu/apsf/
A sympathetic block of the upper extremity is called a stellate ganglia block (SGB). The SGB is performed by inserting a small needle along side the windpipe (trachea). Patients are informed that they
may notice a temporary change in the tone of their voice following the block because some of the local anesthetic may partially numb the vocal cords. They are also informed that they should sip fluids and take small
bites of food immediately after the block. The numbness around the vocal cords temporarily places the patient at a slight risk of coughing in response to drinking and eating. The patient may also notice a temporary
drooping of their upper eye lid due to the SGB (Horner's sign). A sympathetic block of the lower extremity is called a lumbar sympathetic block (LSB). For patient comfort and safety, LSBs should be performed with
the aid of a fluoroscope (X-rays). A video of an LSB being performed can be found on the Web Site for the journal "ANESTHESIOLOGY": 29
To view a 3 minute video of a lumbar sympathetic nerve block being performed.
CLICK HERE
As noted previously in the Guidelines, there may be point-tender spots in the muscles of the affected region due to small muscle spasms called muscle trigger points (myofascial pain syndrome). The patient may obtain
significant relief of the diffuse pain due to RSD/CRPS from a sympathetic block but the pain due to muscle trigger point(s) may persist. Local injection of local anesthetic into the trigger point region and/or application
of physical therapy techniques after a sympathetic block may be necessary to provide further relief of pain.
6. Sympathectomy:
If there is a significant decrease in pain following the sympathetic block, the patient is said to have sympathetically maintained pain (SMP). If there is not a significant decrease in pain, the patient has sympathetically
independent pain (SIP). Only patients with SMP should be considered for a sympathectomy. Patients are advised to expect no more relief of their pain from a permanent block, i.e. sympathectomy, than they received
from either a SGB or a LSB. Thus the patient must really pay attention to the magnitude of pain relief and improvement in function following each sympathetic block. 30-32 Sympathectomy is a relatively invasive procedure with potential complications and should be pursued by the patient only if they are certain about the temporary therapeutic benefits that they received from a series
of SGBs or LSBs.
Recently, laproscopic sympathectomy has been developed for sympathectomy of the upper extremity.33 This technique requires the placement
of three small holes temporarily in the side of the chest wall while the patient is under general anesthesia. For the lower extremity, the patient has the choice of dissolving (destroying) the sympathetic nerves
with phenol injected through a needle while the patient is awake (percutaneous phenol sympathetic neurolysis) or a surgical sympathectomy under general anesthesia. Other techniques for sympathectomy have also been
used. The patient must be informed of the pros and cons of each approach.
Post-sympathectomy pain (neuralgia) is a potential complication of all types of sympathectomy. 4,34 Post-sympathectomy pain is typically proximal to the original pain (e.g. proximal means that the pain may appear for the first time in the groin or buttock region for sympathectomy of the lower extremity and pain
in the chest wall region for sympathectomy of the upper extremity). Patients may think that their RSD/CRPS has spread to a new region after sympathectomy because the pain feels similar to their original RSD/CRPS
pain. The post-sympathectomy pain usually resolves on its own or with 1-3 sympathetic blocks. Thus for some patients, sympathectomy may be a two-step procedure; destruction of sympathetic nerves followed by a sympathetic
block.
Published data35 suggests that sympathectomy in properly selected RSD/CRPS patients may provide one of the most effective treatments for RSD/CRPS.
The selection criteria for sympathectomy are critical in achieving long-term success.
7. Placebo:
The placebo effect (decreased pain due to an inactive treatment such as a sugar pill) must be considered in the treatment of RSD/CRPS. Although the figure of 33% is commonly quoted in papers and textbooks as the percentage
of people who will respond to a placebo, it is misleading because the "percentage" varies enormously (from close to 0 to 100%) depending on the exact circumstances. Physician and patient must have an understanding
about the placebo effect, otherwise the patient is at risk of being over-treated. Recognition of placebo versus specific pain-relieving treatment may be difficult, but there are some distinguishing characteristics.
-
The greater the invasiveness of the procedure itself, the greater the placebo effect. 4,36
-
The greater the expectation for pain relief, the greater will be the placebo effect. 4,36
-
The placebo tends to be of less duration. For example, close monitoring of the patient's pain for hours and days after each sympathetic nerve block has shown that the pain-reducing effect of the saline
(placebo) injection subsides within the first few hours, whereas that of the local anesthetic injection persists for several days. 4
-
The placebo tends to be less reproducible with each successive treatment. 4,36
Therefore, it may be of great potential therapeutic value to provide each patient with a series of multiple sympathetic blocks separated by brief intervals (e.g. one week) simply to determine whether such blocks are effective treatments.
The time-course of pain relief and improvement in function must be monitored closely by the patient. The actual local "anesthetic" effect of a sympathetic block lasts for only a few hours. But patients with SMP
usually experience pain relief that far outlasts the duration of the local anesthetic effect. This type of extended relief of pain and improvement in mobility beyond the duration of the nerve block is believed to indicate
an element of "reflex" activity or a "vicious cycle" in the affected region of the body, either from muscle spasm or from sympathetic over-activity.
Intentional or not, some patients may
not reliably report the effects of sympathetic blocks. As noted, a good sympathetic block provides a feeling of warmth that will act as a "cue." Some patients respond to that change in sensation by anticipating
the results or stating it as a genuinely perceived reduction in pain. Others may deceitfully report pain relief, since they believe that such a report is necessary for further treatment, attention, or other desired
gain. Some patients may feel that some "treatment" is better than no treatment at all, even if the treatment is ineffective. 36
8. Other Types of "Sympathetic Blocks".
A sympathetic blocker (alpha adrenergic antagonist), phentolamine, given I.V. has been advocated as a diagnostic test for SMP. However, false negative tests have been reported as high as 43%. Moreover, this approach is
somewhat elaborate and requires considerable technician time and expense. 4 The phentolamine test is a diagnostic procedure while a sympathetic block is a diagnostic, prognostic
and therapeutic procedure. 37 However, the phentolamine test may be valuable treatment option in the situation where a sympathetic block is not possible or when multiple
extremities are involved.
Epidural blocks are less specific for blocking the sympathetic nervous system and, therefore, they are not as useful for diagnostic and prognostic objectives. The infusion of local
anesthetic through the epidural catheter may cause temporary weakness in the legs, making walking dangerous. Placement of long-term epidural catheters to treat RSD/CRPS still occurs in practice. Perhaps this is because
anesthesiologists are more familiar with the epidural catheter technique than with the selective sympathetic block technique. The long-term epidural catheter approach is more expensive and patients are placed at more
risk for certain rare life-threatening complications, e.g. infection (epidural abscess). Often a short (2-5 days) hospitalization will be necessary to determine the clinically most appropriate dose of the epidural agent
for constant infusion. Dislodgment of the epidural catheter is a relatively common problem. The use of a lumbar sympathetic catheter may provide a more specific sympathetic block than an epidural catheter, but the lumbar
sympathetic catheter is more likely to become dislodged during exercise.5 There is a place for the use of epidural and lumbar sympathetic catheters in the treatment of
RSD/CRPS but the physician should justify these techniques on a case by case basis.
Another technique used to carry out a sympathetic block involves the intravenous injection of sympathetic blocking agents
(e.g. guanethidine, bretylium and clonidine) into an extremity and limiting spread of the agent to the entire body by applying a tourniquet to the extremity.38 This method
requires placing an IV in the painful extremity and may be technically extremely difficult due to severe swelling (edema) of the extremity. The patient may not be able to confirm that they actually received a sympathetic
block because the "cue", a warming sensation in the extremity, may not be felt. Furthermore, there is no evidence that this technique is more effective than the usual sympathetic blocks for the diagnosis and
treatment of RSD/CRPS. The IV tourniquet technique using a sympathetic blocking agent may be considered as an option for patients who must take blood thinners (anticoagulants) where a SGB or a LSB may cause major bleeding.
9. Spinal Cord Stimulation (SCS):
Figure 3 illustrates another method of pain control that works well for some patients with chronic intractable pain due to RSD/CRPS. Spinal cord stimulation (SCS) uses low intensity, electrical impulses to trigger selected
nerve fibers along the spinal cord (dorsal columns), which are believed to stop pain messages from being transferred to the brain. SCS replaces the area of intense pain with a more pleasant tingling sensation called
paresthesia. 39-42 The tingling sensation will remain relatively constant and should not hurt. There is some experimental evidence that SCS may enhance the flow of blood
to the affected extremity by blocking the sympathetic nervous system. 43-45
FIGURE 3
A temporary trial, with a temporary electrode, should be performed first before implanting permanent electrode(s). Given that SCS is a relatively invasive, costly procedure and given that RSD/CRPS patients are often desperate
and frustrated, a baseline psychosocial evaluation that addresses pain management issues should be considered. Although rare, spinal infection and paralysis are potential complications. The ability to insert the electrode
through a small needle has reduced the risk of the procedure and has facilitated the trial with a temporary electrode.
Treating RSD/CRPS with SCS poses unusual clinical and technical problems. RSD/CRPS tends
to be an unpredictable disease from a technical standpoint. The need to focus SCS on the most painful region must be kept in mind, which is more difficult in RSD/CRPS, because the location of the worst pain may change.
Furthermore, the pain from RSD/CRPS may spread to distant parts of the body, requiring multiple successive implanted stimulators to cover the largest possible area. Therefore, even when RSD/CRPS is limited to one extremity,
it is wise to widen stimulation to zones to which the pain might spread.
Because of the risks and high costs of spinal cord stimulation, the treatment is reserved for severely disabled patients. A recent well-controlled
study shows that with careful selection of patients and successful test stimulation, SCS is safe, reduces pain, and improves the health-related quality of life in patients with severe RSD/CRPS. 46,47
The External Battery System Versus the Internal Battery System for Spinal Cord Stimulation
In order to make an informed choice about SCS, the patient and physician should consider the pertinent differences between the internal and external battery systems. In this section, the relative merits of the internal
and external battery systems for spinal cord stimulation are discussed.
CLICK HERE
10. Morphine Pump:
It is well-recognized that a single injection of morphine into the spinal fluid (within the intrathecal space) produces a selective pain-blocking effect on the spinal cord. This selective effect on the spinal cord spares
the patient from many of the serious side effects caused by morphine when it is given orally (e.g. sedation). 36 Soon after this discovery, enthusiasm developed to implant
permanent morphine pumps to treat non-cancer chronic pain, especially after Medicare began to approve this surgical procedure for reimbursement. The implantation of a morphine pump is a relatively invasive and expensive
treatment modality. Despite almost 20 years of testing, no scientific evidence has emerged that long-term use of the morphine pump offers an advantage over oral morphine for treating various chronic pain syndromes,
including RSD/CRPS. In fact, many patients with the implanted morphine pump take oral morphine at the same time. The same complications sometimes associated with oral morphine use are also found with the morphine pump,
such as development of drug tolerance, nausea, constipation, weight gain, decreased sex appetite (libido), swollen legs (edema), and increased sweating. 48-50 In addition,
malfunction of the pump system (dislodgement of the catheter) can be a significant problem. 50
A recent study suggests that with careful selection of patients,
the implantation of a pump for the spinal infusion of baclofen may be a valuable means for treating a certain type of muscle cramp called dystonia in patients with severe RSD/CRPS. 51
11. How to Determine the Effectiveness of Treatments for RSD/CRPS:
Dr. Anthony F. Kirkpatrick, Chairman of the Scientific Advisory Committee, contributed a section to the Clinical Practice Guidelines that focuses on how patients can determine the effectiveness of treatments for RSD/CRPS.
This section is based on Dr. Kirkpatrick's keynote address at RSDSA's Third National Conference, held October 15-16, 1999, in Atlantic City, New Jersey.
CLICK HERE
12. RSD/CRPS in Children

A 30-minute video on RSD/CRPS in children was peer-reviewed by an international panel of experts at the "International Update on RSD/CRPS" held at the University of South Florida, February 1-2, 2002. As a result of the
comments received by this panel, the video was expanded to 43 minutes in order to cover a broader range of issues. During the course of preparing the extended version of the video, it was necessary to consult extensively
with experts in the field of pediatric pain management. These persons included Dr. Sabine Kost-Byerly at Johns Hopkins University, Dr. Robert Wilder at Mayo Clinic and Dr. Robert Schwartzman at Allegheny University
of Health Sciences. To view the video for free:
CLICK HERE
|

