Early April is an exciting time at Baystate Medical Center. That’s when the Springfield, Mass., institution prepares for its annual research week highlighting the latest studies by its 270 faculty members and other scientists.
But 2008 was different. In the run-up to the event, Hal Jenson, MD, Baystate’s chief academic officer, made an alarming discovery. During a routine audit of the summaries, Dr. Jenson found that two abstracts submitted by one of the hospital’s prominent anesthesiologists, Scott S. Reuben, MD, had a potentially critical flaw: neither of the studies appeared to have the approval of Baystate’s institutional review board. That wasn’t necessarily a breach of ethics; after all, multicenter trials often have IRB approval only from sites where patients are enrolled. But it was enough of a red flag that Dr. Jenson asked one of his colleagues to speak with Dr. Reuben about the missing information.
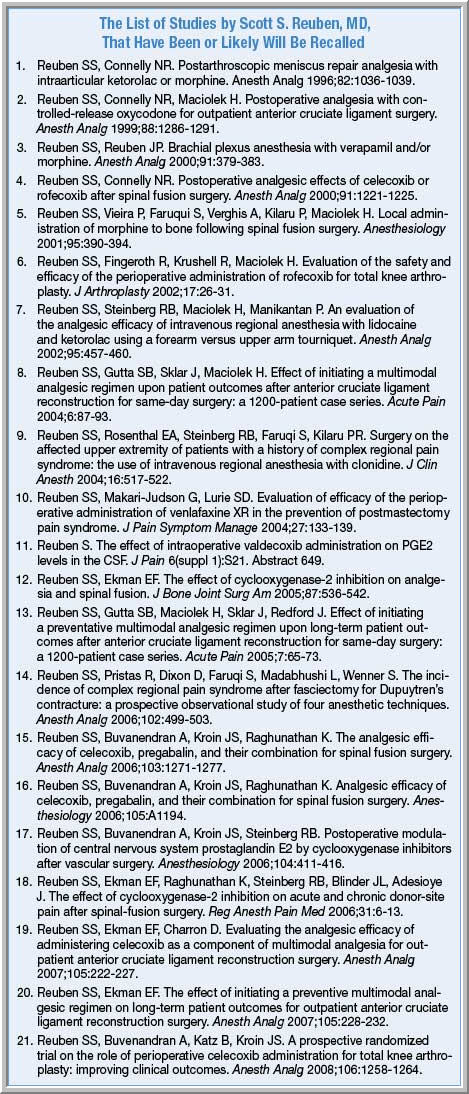
What ensued was the unraveling of what medical ethicists are calling one of the largest instances of research fraud ever reported, a massive scandal that has led to the withdrawal of as many as 21 journal articles (see list).
Virtual Patients
Investigators for the hospital reached a shocking conclusion. “It turned out that was not IRB approval because the data were fabricated because the data were partially or completely fabricated,” Dr. Jenson told Anesthesiology News. Simply put, Dr. Reuben had concocted the data—and in many cases the patients themselves—out of vapor.
Over the following weeks and months, Baystate investigators learned that Dr. Reuben had been falsifying his data for years. A “prolific” writer, according to Dr. Jenson, Dr. Reuben—who graduated from the State University of New York at Buffalo medical school in 1985—has at least 72 published studies to his name on the journal database PubMed, a large number for a relatively young scientist. Yet because of gaps in the record, “in many cases it’s impossible to validate the data for the older studies,” Dr. Jenson said.
Baystate, which earlier this year reached out to the journals involved to request retractions of the suspect articles, stressed that none of Dr. Reuben’s co-authors is believed to have been aware of the fraud. The hospital also insists that no patients were harmed in any way by the deception.
Foundation Weakened
Dr. Reuben’s research helped lay the foundation for an emerging area of perioperative care known as multimodal analgesia. Due to the sheer scope of the misconduct, advocates said, this field now requires major bolstering to regain the confidence of clinicians and researchers. “We are left with a large hole in our understanding of this field,” said Steven L. Shafer, MD, editor of Anesthesia and Analgesia, which has retracted 10 of Dr. Reuben’s papers. “It will take a while for science and practice to sort this out.”
In addition to the charges that he falsified data, Dr. Reuben has been accused by at least two of his co-authors of putting their names on his papers without their consent. One, Evan Ekman, MD, an orthopedic surgeon in Columbia, S.C., told Anesthesiology News that Dr. Reuben “forged” his name as a co-author on two articles in which he had absolutely no involvement. Jane Albert, a spokeswoman for Baystate, said the institution had received a complaint from another researcher who maintains he was not a co-author with Dr. Reuben.
17-Year Career Undone
Dr. Reuben, who began working at Baystate in February 1991, is now on medical leave from his position as director of the acute pain service at the medical center, a private, nonprofit facility affiliated with Tufts University. He also has been stripped of any research and educational activities involving the institutions for a minimum of 10 years, Dr. Jenson said. Under the terms of the hospital’s guidelines for academic integrity, “I have precluded him from presenting the suspect data without my written permission,” said Dr. Jenson, who added that Baystate “does not have any intention of bringing criminal proceedings” against Dr. Reuben in the matter.
Paul F. White, PhD, MD, the Margaret Milam McDermott distinguished chair in anesthesiology at the University of Texas Southwestern Medical Center in Dallas, called the Reuben case “unprecedented in our specialty.”
Dr. White, an editor of Anesthesia and Analgesia, said that given the retracted (and likely-to-be withdrawn) papers and those that are unsullied by the affair, practitioners of multimodal analgesia are now confronted with several significant problems.
Giving patients cyclooxygenase-2 (COX-2) inhibitors such as celecoxib (Celebrex, Pfizer) after surgery has consistently been shown to relieve pain, reduce side effects related to use of opioids and improve the quality of recovery in the early and intermediate postoperative periods. However, Dr. White said, any long-term benefit of these drugs on patient outcomes is unconfirmed.
Another question mark, he said, now looms over “preemptive analgesia” with COX-2 inhibitors and nonsteroidal anti-inflammatory drugs, a component of multimodal therapy that Dr. Reuben strongly advocated. Similarly, doubt has been cast on the alleged lack of adverse effects of COX-2 inhibitors on bone fusion—such as at the spine—an effect Dr. Reuben’s data had supported (although this claim already had been an area of considerable controversy, Dr. White told Anesthesiology News). And finally, he said, whether multimodal analgesia can prevent patients undergoing major orthopedic surgery from developing chronic pain, as Dr. Reuben had argued, remains “unproven.”
Anesthesia and Analgesia will be publishing a series of editorials on the fraud in its May issue.
Because of the layered nature of scientific research and publishing, the scandal “compromises every meta-analysis, editorial, systematic review of analgesic trials”—as well as every lecture and continuing education course—that cited the fraudulent findings, added Dr. White, a member of the editorial board of Anesthesiology News. “Clearly, it’s time get back to the hard work of conducting clinical analgesic studies to address important issues in perioperative pain management and patient outcomes.”
Like many anesthesiologists, Dr. Reuben technically was employed not by the hospital but by a private practice—in this case, Springfield Anesthesia Service, a group of about 50 doctors that contracted with Baystate to work in its operating rooms.
The scandal has left Springfield Anesthesia reeling and embittered. “We’re all very upset about how he strung us along,” said Steven Dunn, MD, a doctor in the practice. “Our group paid him extra money and gave him nonclinical time. We all worked long hours in the OR so that he could do his research.”
Dr. Dunn said he was a co-author with Dr. Reuben of one study, but because he collected the data on that paper himself, the results have not been challenged. However, he said, the nature of the fraud was surprisingly simple—and difficult to detect. “You can see how easy it was to get away with,” he said. “If someone comes to you and says, ‘Here are data on seven patients,’ how do you say, ‘No, I didn’t see you treat those patients’? You assume that a physician would have the integrity not to lie in this way.”
Dr. Dunn, who has neither seen nor talked with Dr. Reuben since the fraud was discovered, said he hoped the scandal would not diminish the reputation of Baystate, which he called an “excellent quality” institution. “Baystate has handled this situation in a forthright and proper manner since the initial discovery. It’s disheartening for us that some guy would do this,” he said.
The most alarming aspect of the episode for him, Dr. Dunn said, was that as a skeptic of multimodal analgesia, he would frequently find himself in debates with Dr. Reuben about the approach. During one of those exchanges, Dr. Reuben presented his colleague with a study whose data were so convincing that Dr. Dunn began to doubt his stance. That paper, he recently learned, was on the list of articles to be retracted. “I was appalled that someone could take a paper based on fraudulent work and try to change my practice,” he said.
|

 is well-known among anesthesiology researchers for his studies of multimodal analgesia, the practice of combining several forms of pain relief to better control postoperative discomfort and promote faster recovery from surgery.
is well-known among anesthesiology researchers for his studies of multimodal analgesia, the practice of combining several forms of pain relief to better control postoperative discomfort and promote faster recovery from surgery.