Part I: MEASURING PAIN OBJECTIVELY
PART I
PART II
Participants:
Humberto Sainz Cabrera MD
Alberto Martinez MD
Anthony Kirkpatrick MD Ph.D
Hannah Williams (19-year-old Patient)
Dad (Patient’s father)
Mom (Patient's mother)
Location:
The National Hotel
Havana, Cuba
Date:
March 20, 2015
PART I:
On March 20, 2015, Anthony Kirkpatrick M.D., Ph.D. was invited to present a 1-hour lecture on complex regional pain syndrome at Cuba's National Hotel in Havana. The lecture focused on how to measure pain objectively in patients with this neurological disorder.
During the lecture, Dr. Kirkpatrick presented a 19-year-old patient with complex regional pain syndrome. The patient's 3-month follow-up evaluation is presented in Part ll below. |
Click here for video

DR. KIRKPATRICK: Let's begin by talking about reflex sympathetic dystrophy.
Reflex sympathetic dystrophy is the old name for this disease.
Now everybody wants to call it complex regional pain syndrome.
It is the same thing.
Let's begin by speaking about that disease. By the way, Alberto please remind me "despacio" , to slow down if necessary

There are other disease states that are similar to reflex sympathetic dystrophy.
The big one is fibromyalgia.
Another disease which is not pain but is a pain in the head "Mucho Mucho dolor". It is called depression.
Intractable depression.
It is worse than pain in a way because the lights in the head never come on. It is dark in the head all the time.
We know that ketamine can be effective in that situation as well.
But we're going to focus today on the complex regional pain syndrome.
We are going to focus on how to measure pain.
People say that pain is only subjective.
How can we rely on that?
If I come to Humberto, and he has a big white coat on and he looks like a professor, and he does just look at him.
You should get a picture of him over there.
Patients do not want to tell you the bad news.
They do not want to say that they came all the way from the United States to get their pain treatment, and it did not work.
They do not want to do that.
So what we try to do at the Foundation is base everything on objective analysis.
The objective analysis is in terms of pain and let’s not forget in terms of strength and range of motion as well.
Therefore, what we want to focus on today is the measurement of pain objectively.
The first thing I need to do is to tell you what this thing is called complex regional pain syndrome.
You must remember that it is a clinical diagnosis.
What do I mean? There is no laboratory test for the disease.
But you can get a pretty objective picture if you're dealing with RSD if you have the right tools.
For example, let's talk about the clinical history.
There are three criteria.
Criteria #1 is when the injury does not follow the normal expected healing course.
For example, if you get a sprained thumb. Within a week, you expect the swelling to go down and the pain to decrease.
But if the pain is increasing, especially if it turns into a burning pain, and if the pain is spreading from the arm into the face or down into the legs.
The patient is either crazy or they have RSD.
Now we are getting into one of the challenges of dealing with this disease.
Because it is true that some of the symptoms that the patient describes sound like they're crazy.
So you as a doctor have to distinguish between the subjective symptoms described by the patient in emotional terms and the diseased state.
So one of the things that help in making the diagnosis of RSD is the fact that it involves the sympathetic nervous system.
So the second criteria, in addition to not following the normal healing course, is that there is an abnormal function of the sympathetic nervous system which can be measured.
As doctors, you know that the sympathetic nervous system controls the flow of blood.
For example, controlling the flow of blood flow in the skin.
For example, you're walking along, and you step on some glass.
It's an emergency.
So the sympathetic nervous system causes the blood vessels in the skin to contract so that you don't spill blood all over the place.
So if you are in Cuba, and the police are chasing you down the street, your sympathetic nervous system is activated so that blood is diverted into your legs so that you can run faster.
The same type of emergency response to police would happen in the United States as well.
So it's an emergency response.
So what does that mean physiologically?
It means that the sympathetic nervous system is activated on both sides of the body symmetrically.
But with RSD the sympathetic nervous system functions asymmetrically.
This is a very important concept.
The right leg that stepped on the glass may be colder, or it may be warmer.
That's why measuring temperature of the skin objectively using an infra-red scanner is important.
That's why this infrared scanner that I'm showing you is important.

So now if we take Alberto here who has never been tested before, and measure his skin temperature, we can show that he is still alive.
However, Dr. Alberto your skin temperature is slowly decreasing indicating that you are slowly dying.
So you're looking for things like asymmetrical temperature changes, asymmetrical sweating in the body, asymmetrical swelling in the body.
So all these asymmetrical changes suggest objective evidence of reflex sympathetic dystrophy.
Everything I'm telling you about the diagnostic criteria is documented in the scientific literature.
The third criteria is that you have to rule out other possible explanations for the observed signs and symptoms of the disease.
For example, a woman who has swelling and a cold extremity on one side could have breast cancer.
Keep in mind that RSD is far more common in women than in men. The distribution is about 60/40 in adults. And children it is far more common in little girls.
The important thing to remember is to look for the asymmetry on the two sides of the body.
If you see the asymmetrical changes, you know that you're probably not dealing with a symmetrical disease such as rheumatoid arthritis.
You have to be able to make a good differential diagnosis.
Let's stop talking about the diagnosis of RSD.
Now let's turn to how to measure the clinical outcome in patients with RSD on an objective basis.
The challenge that pain is a perception.
For example, some studies show that some cultures cry easier when subject to pain than other cultures.
Gender may play a role in certain cultures in terms of perceiving pain.
But for some disease states we can measure pain objectively such is the case for RSD.
How do we do that?
We know that parts of the body, especially where the body has been injured and have spread, is far more sensitive to the application pressure. So these patients say ouch much faster than patients who do not have RSD when their finger is squeezed.
Well, take advantage of that.
You can take a device that looks like this.
And we put pressure on the skin.
Dr. Alberto was asking me earlier how accurate is this device.
More importantly, how precise is this instrument.
There is a difference between accuracy and precision.
So how precise is this instrument?
We have not done this test before on Alberto.
We are going to see how precise this is on Alberto.
When the pressure sensation turns to pain, you are going to say stop.
You are not going to look at the numbers.
You're going to say stop, "parar"

So everybody knows that was a 3.5.
(10 minutes and 15 seconds into the video)
So everybody knows that was 3.5 kg.
Is that correct?
DR. CABRERA: That is correct.
DR. KIRKPATRICK: What's that number?
DR. CABRERA: 3.5.
DR. KIRKPATRICK: Are you ready for the last one?
Always do three measurements.
Dr. Humberto what is that number?
DR. CABRERA: 3.5
DR. KIRKPATRICK: That's what we call precision.
DR. CABRERA: May I?
DR. KIRKPATRICK: Of course, this is what we call a controlled study.
I have to do a couple of practice tests so you will know what I'm talking about.
So when the pressure sensation turns to pain, you're going to say stop. That's what we call a pain threshold.
This is a practice one.
DR. CABRERA: Stop
DR. KIRKPATRICK: Are you ready for the real thing?
DR. CABRERA: Stop
DR. KIRKPATRICK: What is that number?
DR. MARTINEZ: 3.25
DR. CABRERA: Stop
DR. KIRKPATRICK: What is that number?
DR. MARTINEZ: 3.5
DR. CABRERA: stop
DR. KIRKPATRICK: What is that number?
DR. MARTINEZ: 3.25
DR. KIRKPATRICK: What does that mean?
That means that he is a bigger baby than you are.
You can handle more pain that he can.
The point I want to make is that if you look at this in terms of scientific measurements this is a precise measurement.
So this is a valuable tool.
Now let's show you how this is used in a patient.
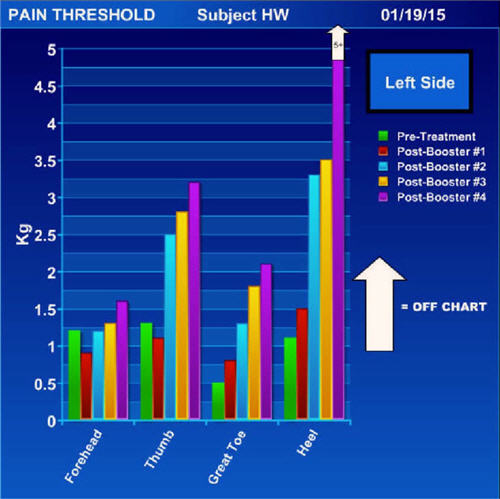
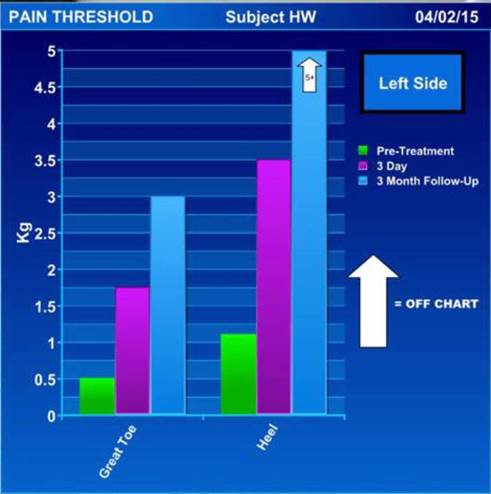
(Dr. Kirkpatrick displays a pain threshold graph)
This graph is her left side.
This is how much pressure was required to trigger pain before we treated her with ketamine.
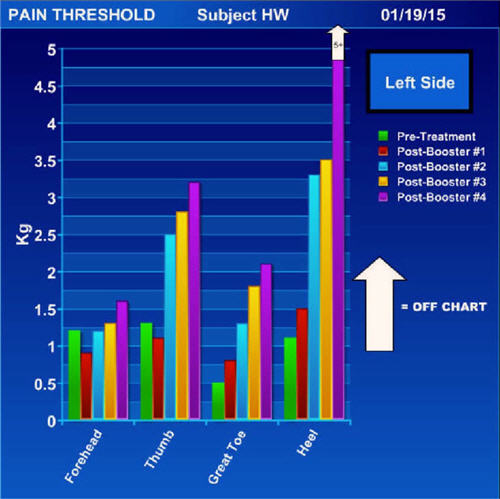
After four days of treatment with ketamine, she is off the scale.
It takes far more pressure on her left heel to trigger the pain.
You see a similar result for her big toe.
You can also see that her RSD is not just in her left leg where she was injured, but it is also in her left upper extremity as well.
What does that tell you?
You have just witnessed how precise this measurement is.
You know as a doctor that you helped the patient.
You don't know what to believe when the patient tells you that you are the greatest doctor since 7-Up was invented.
You just don't know.
The patient might just be patronizing you.
Why is that important? Because as a doctor you want to know that you are helping the patient.
If those numbers were going down, you know that you were not helping the patient.
Maybe you need to rethink two things.
First, maybe you did not get the right diagnosis.
Second, maybe this treatment does not work.
You as the doctor need to have the assurance that you are helping the patient.
The patient needs to know that you are helping them.
Recently, I had a husband tell me that he does not know if his wife is doing better after a ketamine treatment.
I show him these objective measurements, and they say "holy crap."
Is crap a word in Spanish?
You know, and the patient knows that you help them.
You can show them these measurements and feel confident that you have helped the patient.
This is just one parameter. This is just one parameter that you can use to demonstrate that you have helped the patient.
Now we're going to move onto another parameter that is very important.
You have a patient who comes in and says I got the RSD in my leg doctor but I can't comb my hair, I cannot brush my teeth.
And you say to yourself, she has the RSD in her leg, but how can it affect her head?
So you do the pain thresholds, and you find that the pain thresholds are not only lower in her leg but also lower in her head as well.
The Foundation has done pain thresholds in normal people, so we know when we see these low measurements in the head that they are indeed abnormal pain thresholds.
Another way to measure pain objectively is by measuring movement.
The patient says that they cannot feed themselves.
So you measure movement in their hands before and after treatment.
Now I'm going to show you an example of that on video recording of a patient.
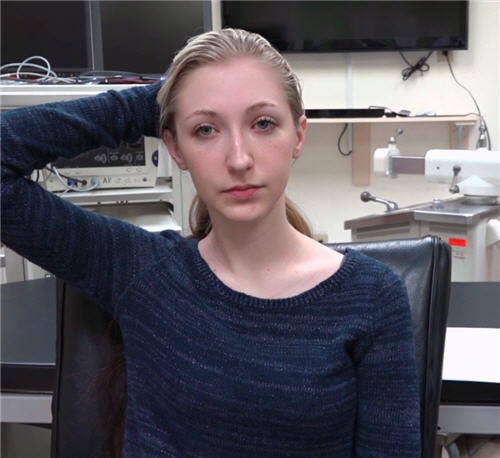
This is a young 19-year-old girl.
RSD is far more common in women than men, for example, usually between the ages of 20 and 30 years.
Keep in mind as you watch the video that there is a certain amount of doctor-patient relationship that goes on during evaluation.
What do I mean by that?
These patients are scared. Many have been suffering in pain for years. They don't know this Dr. Kirkpatrick. Who is he? What you will see here is how I interact with patients. Some of it is kind of goofy. I tease them. I played with them a little bit. I get them to relax a little bit. They are scared, they are frightened. None of the treatments have worked. And who are you? Are you just another one of those doctors who have failed to fix the problem? This is the way I interview. It may not work for you, but it works for me.
(Dr. Kirkpatrick plays the video of the patient)
DR. KIRKPATRICK: Today is January 12, 2015.
Let's go over your history a little bit.
Approximately a year and a half ago you had a relatively minor injury to the left lower extremity involving the foot.
No fractures were involved. Shortly thereafter you were diagnosed with reflex sympathetic dystrophy. There have been several options discussed including but not limited to epidural injections and local injections. We talked about the fact that if you have a complex regional pain syndrome that the local injections can make your pain worse.
Let's ask you a question. Have you given this a lot of thought, correct?
What made you come to the conclusion that this was the best option for you?
HANNAH: I didn't feel that there was any other option that would work as well as this one. I tried other things such as medication and no progress. Things have just been getting worse.
(Dr. Kirkpatrick interrupted the video to make a point to the doctors)
DR. KIRKPATRICK: Let me interrupt the video for a minute. One of the things you have to do as a doctor especially in the United States, and I do not know how it is done here in Cuba, is to provide informed consent. You want to make sure the patient decided to go ahead with this procedure, after giving it careful thought. This patient did not come in the day before the procedure to make this decision. She came in a week before for an initial evaluation. And now I'm asking her one week later why she decided on this treatment. What she is going to tell you is doctor it is no longer in my leg. It is in my arms it is in my face, I can't eat. I cannot open my mouth very well.
I have documented on the video that she understood these things.
In the United States malpractice is a big problem.
Mucho, Mucho problema.
Remember what I am going to do to the patient.
Martha come over here with the video camera.
What I'm going to do is give her ketamine. What I'm going to do is cut off her head. There are going to be no signals coming from below the neck to the brain. That's what ketamine does. It is called dissociative anesthesia. So I want to make sure that this patient and her family understand what she is getting into.
The patient is 19 years old. In Cuba, I think it is the same as in the United States. Consent is when you are 18 years or older. Is that true in Cuba as well?
DR. CABRERA: Here it is 18 years and 29 days.
DR. KIRKPATRICK: I want to make one other point. The patient is 19 years old, and her parents are there. In the United States, it may be considered a criminal offense if you disclose, without the patient's consent, personalized health information. You will see later on in this recording where I asked the family if they are okay with me using this video recording for educational purposes. Let's return to the video.
DR. KIRKPATRICK: The CRPS, based on all the measurements that we have made on you indicates that the disease is not just in your left lower extremity but is diffuse throughout your entire body.
What ketamine does is that it treats the whole body. It is not just treating that isolated part of your body. As the nerve blocks would do, for example.
Are you ready to do some measurements so that we can determine where you started before treatment with regards to strength and range of motion?
Let's do the vertical finger test by placing two vertical fingers in your mouth.
I'm going to ask you if you have any pain when you do that in your face.
Are you having any pain when you do that?
HANNAH: Yes and it's worst on the left side of my face.
DR. KIRKPATRICK: Put the right hand behind your head as best you can. Are you having any pain when you do that?
HANNAH: No
DR. KIRKPATRICK: Now do the left hand behind your head. Any pain when you do that?
HANNAH: no
DR. KIRKPATRICK: Put your right hand out in front of you and open and close it as fast as you can. Are you having any pain when you open and close your hand?
HANNAH: no
DR. KIRKPATRICK: Does your right hand feel stiff?
HANNAH: yes
DR. KIRKPATRICK: Now do the same with your left hand. Are you having pain when you do that?
HANNAH: yes and it goes above my wrist. It also goes above my elbow.
DR. KIRKPATRICK: Now I want you to take both hands out in front of you and open and close them as fast as you can.
Do you notice how stiff the hands are especially on the right side?
HANNAH: yes
DR. KIRKPATRICK: Previously we marked you where you had allodynia in the left lower extremity. Allodynia means that any tactile stimulation is perceived as being painful. The pain will feel like a road burn sensation.
Stop when the light stroking of your skin starts to feel like a road burn sensation. Keep your eyes closed as you lightly stroke your skin. Good job.
Next I want you to take the right foot off the ground, and I want to rotate your ankle. Did you have pain when your rotated your ankle?
HANNAH: yes and it radiated up my foot to my hip area.
DR. KIRKPATRICK: Now do the same thing for the left foot. Did you have pain when you did that?
HANNAH: Yes -- it radiated from my foot to my hip, and it was much worse on the left side compared to the right.
DR. KIRKPATRICK: I do not want you to torture yourself, but it is important that we get an idea of what you can and cannot do. Please be careful not to fall.
I want you to take three steps forward and then three steps back.
Where did you have the pain when you try to walk?
HANNAH: The pain radiated from my feet into my hip region. It was far worse at my left lower extremity.
DR. KIRKPATRICK: Now I want you to try as best you can to take three steps forward on your toes and then three steps back on your toes.
Okay, I get the idea. You cannot do it.
Now I want you to try the same three steps forward and three steps back on your heels.
There is one thing that I want both of you to appreciate is that after your pain was stimulated it doesn't resolve right away. In fact, it can last for hours. Do you agree with that Hannah?
HANNAH: yes

DR. KIRKPATRICK: Dad, I want you to tell me how this is impacted on the quality of her life.
DAD: She was doing everything that a normal 17-year-old was doing prior to this accident. Since the injury to her left foot, this has been an ongoing battle with pain. It went from her foot to travel throughout her entire body. She has tremors and seizure-like body movements. Shaking badly.
DR. KIRKPATRICK: The tremors and seizure-like movements are a natural body defense to severe, unbearable pain. This is a natural body defense that we all have, even if we do not have RSD. This is something that Hannah has no control over.
How do we know that? Take, for example, the Japanese, who held American prisoners of war. What they would do to these prisoners, and I'm going to put it bluntly, they tied piano wires around their testicles to torture them in pain to get them to talk. They would torture them that way. What the prisoners would do in order to get through the unbearable pain from torture, they would have body movements like tremors, seizure-like movements and even paralysis similar to what you described for Hannah. That was the way prisoners protected themselves from their brain being overwhelmed with pain. It is something that we are all capable of, and it is a natural body response to unbearable pain.
We see this type of movement disorder a lot in patients with CRPS, especially in young people.
Doctors are often baffled by these movement disorders. They often accuse the patient of faking their pain.
DAD: We recognize that she is in severe pain and has been so for a long period of time. We know definitely that the pain is real. She is hardly able to do anything. She cannot do any extracurricular activities. She cannot go out and have fun.
DR. KIRKPATRICK: Does that pretty much tells a story Hannah?
HANNAH: Even walking to the bathroom to take a shower I need help. Just washing and the pressure of the shower is painful.
DR. KIRKPATRICK: Some people, like Hannah, who have CRPS in their face cannot even shampoo their hair without having pain. Some patients go ahead and just shave their head of hair.
DAD: There are a lot of times when she can't even stand to have her clothes touching her body.
HANNAH: Even the bed sheets are painful.
DR. KIRKPATRICK: At this point do any of you have any questions?
DAD: no
HANNAH: no
(Dr. Kirkpatrick transitions to address the doctors at the conference).
DR. KIRKPATRICK: I want to focus today on the objective measurement of outcome.
We are going to go to the next video and show you what it's like when she's under the influence of ketamine.
How do we keep these patients safe?
We want to safely reboot the brain.
Dr. Humberto when you have a problem with your computer what do you do?
What do you do when you cannot figure out what is wrong with your computer?
DR. CABRERA: I do a restart.
DR. KIRKPATRICK: That's what we're doing with the brain. The brain is essentially the same as a computer. They say it takes about half a watt or more to run the brain. It takes electricity to run the brain. We shut the brain down and let it come back online again. This is done repeatedly over a four-day period. So you may ask are we doing the infusion of ketamine constantly day and night? The answer is no.
What you need to understand is that ketamine inhibits a substance called glutamate. What the hell is glutamate? I will tell you what it is. If you do not have glutamate, you do not feel pain. Children born without glutamate, usually die at 5 to 10 years old. They usually bleed to death without knowing it. They do not know that they cut themselves.
Patients who get complex regional pain syndrome or fibromyalgia have elevated levels of glutamate in the spinal fluid. What ketamine does is that it inhibits glutamate.
It should not surprise you therefore that by giving ketamine you will decrease the patient's pain.
But what is surprising, is that pain relief can last for months.
The ketamine is gone, it is redistributed throughout the body and eliminated.
Here is what is important. If you give ketamine the first day for four hours and you don't give it the following day, the glutamate levels climb back up.
So what we do over four days, is decrease the ketamine down to this level, and then down to this level, and then down to this level, until we get it very low.
That's why we do not have to put patients in a coma as much as we used to in the past.
Before we had to put the patient in a coma in the intensive care unit for five days with a constant infusion of massive doses of ketamine. This cost "Mucho Mucho Dinero". "Muy, muy caro". Now, that is not necessary. We do have patients we have to put in a coma because they are too sick. We cannot treat them on an outpatient basis with ketamine.
We have determined from our testing that it takes about four days to get the glutamate levels down to an adequate level. You're going to see in this next video what it is like when the patient is under high dose of ketamine on an outpatient basis.
How do we keep the patient from going into a coma. It is very simple. We asked the patient questions every 15 minutes while they are receiving ketamine. We want to make sure they have their long-term memory but lose their short-term memory.
The first thing that gets knocked out with ketamine is your short-term memory. Let me give you an example. I'm going to pick on Alberto now. Are you ready? Can I ask you a question? What country do you live in?
DR. MARTINEZ: Cuba.
DR. KIRKPATRICK: So that's part of your long-term memory. It is burned into that disk in your brain.
May I ask you another question? I notice under the door that there is a red marble. Can I ask you a question? What did I notice under the door?
DR. MARTINEZ: You notice that when you came in?
DR. KIRKPATRICK: What did I notice under the door?
Can I ask you another question?
I noticed that the doorknob over there is green.
Can I ask you a question? What did I notice about the doorknob over there?
DR. MARTINEZ: The doorknob is green.
DR. KIRKPATRICK: When you are under the influence of ketamine you cannot answer that question. It is part of your short-term memory.
You do not have to be a doctor to ask the question and get an answer. A family member can ask the questions.
Here is what it's like for the patient after being under ketamine for four days.
(Dr. Kirkatrick begins the video of the patient again).
DR. KIRKPATRICK: Hannah were going to do some testing on you.
It is January 16, 2015.
She's been on 200 mg of ketamine per hour.
Her vital signs have been very stable. Breathing has been great. She had no adverse hallucinations.

She has had excessive secretions of saliva which does not surprise us given her young age. We have been able to control her saliva with the use of Robinul.
Hannah, your dad needs to ask you a couple of questions.
DR. KIRKPATRICK: That lip movement is typical of what we see when patients are on high doses of ketamine.
DAD: What is your dad's name?
HANNAH: Chris.
DAD: what is your mom's name.
what is your dogs name?
HANNAH: Emily.
DAD: what is your boyfriend's name?
DR. KIRKPATRICK: She has lost her short-term memory and that explains why she cannot remember her boyfriend's name.
Mary has got some questions for you.
MARY: Hannah can I ask you a question?
HANNAH: yes.
MARY: Hannah I noticed that your dad is wearing green glasses.
Hannah can I ask you a question?
What did I notice about your dad?
MARY: hi Hannah.
HANNAH: hi
MARY: Hannah I noticed that your dad is wearing a pink shirt.
Hannah can I ask you a question?
What did I notice about your dad?
DR. KIRKPATRICK: She can answer the long-term questions but not the short term questions.
Which is very good
.
(Dr. Kirkpatrick returns to the conference in Havana Cuba)
DR. KIRKPATRICK: What you have learned is that she's lost her short-term memory but her long-term memory seems to remain in tact.
The patient has some brain function left but not much.
If I ask her to take a deep breath she will take the usual deep breath.
Each ketamine infusion is for four hours.
You might ask: Tony, why is she not under general anesthesia?
I will tell you why.
Because we started low with the ketamine dose and gradually worked up on the dose.
It was not an induction dose of ketamine for general anesthesia.
The other question is why didn't she have adverse hallucinations?
"Muy muy importante"
You notice that the father is by her bedside.
Someone who is familiar to the patient in her long-term memory must be in the room with her.
This is huge at preventing the patient from slipping into an adverse hallucination.
And she is not asleep.
Usually when a patient has an adverse hallucination, they doze off. And then "boom" they have an adverse hallucination.
Why is it so terrifying when you are asleep?
Let me give you an example.
You are here today at the National Hotel. You wake up and you have a bad dream. You're at your home and your wake up and have a bad dream. Where would you rather be at this hotel or at home.?
DR. CABRERA: I would rather be at home.
DR. KIRKPATRICK: Of course, you'd rather be at home. You wake up you see the ceiling fan, so you know you are safe. So it is important to keep the patient awake. Do not ever do high doses ketamine without having a significant other person in the room that the patient trusts.
By the way doctors, this takes a huge workload off of you. Guess who is by the bedside during the ketamine infusion.? Who is measuring her cognitive function? It is not me. It's the father or it's the mother and it's less work for you. It means that you can do other things with your time.

"Qué pasa Martha?"
MARTHA: you said "boom".
DR. KIRKPATRICK: Is she falling asleep?
DR. MARTINEZ: you said boom, that must've scared her.
DR. KIRKPATRICK: Did I scare her?
Martha, Sauve, Sauve, Sauve,
Martha like this like this.
Now we're going to take a look at how the patient responded to her treatment in terms of her function.
Again, this is another independent parameter or measurement that we can make on the patient to measure her outcome objectively.
DR. MARTINEZ: How long does it take to recover from the ketamine infusion?
DR. KIRKPATRICK: Alberto is asking an important question. So let me respond.
Ketamine has a very rapid re-distribution half-life.
So what does that mean in simple language?
When you turn the ketamine infusion off, it leaves the brain quickly.
Very quickly.
Very quickly like "boom" she's awake almost immediately when you turn the ketamine off.
Let's talk about some of the potential adverse effects of ketamine.
You saw the patient with excessive salivation. You have done children with the use of ketamine and you have probably witnessed the same problem with excessive salivation.
They drool all over their face. So we have Robinul or glycopyrrolate in the United States. We give them a 0.2 mg of Robinul and this can control excessive salivation.
So if I don't use glycopyrrolate the salivation comes falling down to the floor. Then you start sliding all over the floor. Dr. Humbert all goes, Tony you're exaggerating. I'm exaggerating only a little bit:
"Un poco"
DR. CABRERA: I have been using ketamine for many years and I know about the problem with excessive salivation. We sometimes use atropine.
DR. KIRKPATRICK: I prefer not to use atropine because of its effects on the heart.
What else bad can happen with ketamine?
Nausea and vomiting can be a problem especially in women. Dr. Humberto you know how women are right?
DR. CABRERA: Usually. Hormone dependent.
DR. KIRKPATRICK: With some women no matter what you give them they can get nauseated. They get nausea and queasiness much easier than men. You just take the bottle of ketamine and wave it in front of them and they get sick. The thought of ketamine can cause a woman to feel nauseous.
My point is this. Nausea and vomiting is something that can happen. Therefore, you make sure that the patient is adequately hydrated. If the patient is that way, you make sure you give them some medication as a prophylactic before you start the procedure. You can give the patient Zofran about an hour before they come in for the ketamine procedure. 24 mg orally one hour before they come in for the procedure is a good dose.
During the infusion a drug that is very useful that has been around for decades is Decadron or dexamethasone. It works fantastic for nausea and vomiting
DR. CABRERA: Or you can give the patient a low dose of droperidol.
DR. KIRKPATRICK: Yes you can give droperidol to her but it can cause some adverse effects on the brain. You don't get that effect with Zofran. And dexamethasone is not that expensive.
I recommend dexamethasone because it has virtually no side effects when given.
What dose do I give in such circumstances? 12 mg of dexamethasone by IV push.
Do you know what is fascinating about dexamethasone? If you give dexamethasone too fast, it will cause pain in the groin area. What the hell causes that? I don't know. But it happens. So therefore you give the dexamethasone slowly by IV push.
Another point I would like to make about adverse effects is that we rarely ever see adverse hallucinations. When Dr. Schwartzman and I started using ketamine to treat complex regional pain syndrome over a decade ago, we had a serious problem with adverse hallucinations. Patients were tearing out there IVs, yelling and screaming, and doing all kinds of terrible things. We hardly ever see that anymore.
"No mas!"
If the patient has an adverse hallucination, you can give them more midazolam. But try to stay away from midazolam. If you give midazolam at the beginning of the infusion, no problem. The more midazolam you give the more the patient is likely to slip into a deep anesthesia. That means you will be unable to give them an optimal dose of ketamine under those circumstances.
Let's move on and see how the patient did after her treatment with ketamine.

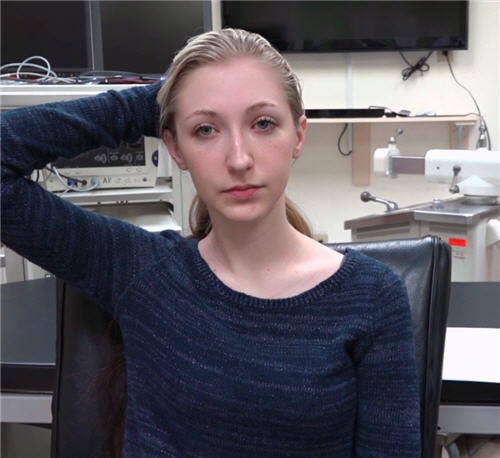
DR. KIRKPATRICK: Okay Hannah, today is the 19th of January and that means it's about 2 to 3 days after your last ketamine infusion which was on Friday.
HANNAH: Yes
DR. KIRKPATRICK: And we just did your pain thresholds, and of course there is a dramatic improvement in your pain thresholds. What we're going to do is talk about how things went during the infusion.
So you were there dad. Mom was there, and the whole family was there.
We did run into an issue with some queasiness and nausea.
As you know she has a history of migraines and that doesn't surprise anybody, okay?
But we were able to get it under control with giving her some Zofran before she came in, orally, and she had some Decadron during the procedure as well as some glycopyrrolate or Robinul which keeps her from accumulating a lot of saliva. Excessive salivation can be extremely uncomfortable if you're under the influence of ketamine, but we got it under control. Would you agree to that?
HANNAH: Yes
DR. KIRKPATRICK: You didn't have any adverse hallucinations during the treatment right?
HANNAH: Right
DR. KIRKPATRICK: So that wasn't a problem The one thing that limited us was that you would go into a deep anesthesia. You had difficulty answering questions and we're going to go over that with you a little bit in more detail in a minute, okay?
So, but we got you up to 200 mg of ketamine per hour so that's a very good dose. Are you ready to do some exercises to see what happened with you?
HANNAH: Yes
DR. KIRKPATRICK: Okay let's do the vertical finger test. Look straight ahead, don’t look at me. Put two vertical fingers in your mouth. Are you having any pain when you do that?
HANNAH: No
DR. KIRKPATRICK: Remember, you had pain on the right side of your face and worse on the left side of your face than on the right side of your face. You don’t have that now?
HANNAH: No
DR. KIRKPATRICK: Take that right hand; put it behind your head please. Any pain when you do that?
HANNAH: No
DR. KIRKPATRICK: Didn't have that when we started, don't have one now.
Now put the left hand behind the head. You didn't have any pain there when you started and you still don't, is that correct?
HANNAH: Yes
DR. KIRKPATRICK: Now take the right and put it out in front of you. Open and close as fast as you can. Less stiff huh; it's much faster, isn’t it? Any pain when you do that? You didn’t have pain when you started, don't have it now right?
HANNAH: Right
DR. KIRKPATRICK: You did have pain when you tried to do that on your left side.
Go ahead and open and close as fast as you can. Much faster now isn’t it? And do you still have that pain up around your thumb and your finger?
HANNAH: No
DR. KIRKPATRICK: And you don't have that now. Put both hands in front of you. Open and close as fast as you can, much faster now huh? So, are you going to start to play the piano, is that what you’re going to do?

MOM: violin
DR. KIRKPATRICK: Violin?
DAD: She plays violin.
DR. KIRKPATRICK: Is that right? That was before all this happened she was doing that?
DAD: Yes
DR. KIRKPATRICK: That's interesting, very interesting. Okay now the next thing we are going to do here is, we're going to ask you to roll up that pant leg on your left side here, and we have these marks on you where you had the Allodynia.
Now it’s real sensitive skin; felt like road burn before we started so I want to test that now to see if that disappeared. So go ahead and start above that black mark, close your eyes so you don't cheat, perform light stroking of the skin and see if you still have any of that road burn sensation. Feel that down there anymore?
HANNAH: No
DR. KIRKPATRICK: Okay go down the other side there now. Okay there you go. All gone.
HANNAH: Yes
DR. KIRKPATRICK: Excellent.
Now the next thing I want you to do, I want you to rotate that right ankle for me please. There you go, it’s less and less stiff there isn’t it?
HANNAH: Yes
DR. KIRKPATRICK: Any pain when you do that?
HANNAH: No
DR. KIRKPATRICK: Now do the worst side, which is your left side. Go ahead and rotate it.
Any pain when you do that?
HANNAH: No, not really.
DR. KIRKPATRICK: And listen, while we are on that subject, remember we talked about the fact that you haven't been walking and you're out of shape right?
It's not your fault that just happens to everybody especially if it’s in a lower extremity. We're going to talk more about how to get rid of that, what we call muscle pain.
That's not RSD pain. We’ll talk about that later.
But you notice just how much better the range of motion you have down there.
You move that foot a hell of a lot better than you did before.
Wiggle your toes for us. Alright, can you hitchhike back to plant city? Ah, look she can do it! Alright, very good, excellent.
Let’s stand by the door there. Dad is going to be by your side just as a safety precaution ok?
MOM: The color is better too.
DR. KIRKPATRICK: Yes, well it's going to improve a lot more than it is right now with the exercises. She’s got to re-establish her circulation down there in those legs okay?
Go ahead and take three steps forward please? Just regular walking. That a girl. You’re much more secure now aren't you?
HANNAH: Yes
DR. KIRKPATRICK: Go on back please. There you go. Remember you had pain going all the way up to your hips when you did that before. What's going on now?
HANNAH: Not the same kind of pain
DR. KIRKPATRICK: It's more of that muscle pain from just being out of shape, right?
HANNAH: Right
DR. KIRKPATRICK: Okay and that's the kind of pain you can live with. You can't live with the pain that sucks your breath out, right? It takes your breath away, okay.
Now the next thing I want you to do, you couldn't even do this before, but see if you can take three steps forward on your toes. Your dad is there if you need him for balance. Okay see if you could do that now. One, two, and three. Very good, good job.
Now did that give you the same pain you had before?
HANNAH: Yes
DR. KIRKPATRICK: Is it the same pain?
HANNAH: Oh no not the same as the RSD.
DR. KIRKPATRICK: Right, right, now listen, we talked about another thing didn't we? We talked about the fact that you’ve got to learn how to walk again. Remember you have not been walking, okay, so it's going to take a while, like anybody, to pick that up again and try to walk, okay.
Now the next thing we're going to ask you to do for completeness - see if you can walk on your heels. Go ahead. One, two and three. That's good and again do you still have the pain you had before we treated you
HANNAH: No
DR. KIRKPATRICK: No, okay. Have a seat please. Alright, now let's go over the treatment plan here. Again if there is something you do not understand just interrupt me and we’ll get it clarified, okay.
Alright. Now we talked about the heated pool exercises three days a week no more than 20 minutes each time. The water temperature should be between 82 and 86°F.
We talked about getting yourself one of these little digital thermometers, you know, that you can use that will help you with gauging whether you should even get in the water. So if it's 80 or 81° you probably don't even want to go in the water that day okay.
Now the other thing we talked about is the four reasons why this works:
Reason one is you're not ready for full weight-bearing. In fact it's kind of risky because you could fall and re-injure yourself which is the most common reason why patients have a relapse
Okay. Number two: the water is a very, very potent desensitizer, so it will even desensitize your skin so you could tolerate touch better than even now, ok.
And the third thing we talked about is many times over and over again you need to avoid exercises that can result in re-injury, okay, and water is an exercise you can do where you are least likely to re-injure yourself.
And the fourth thing we talked about is this thing called stress, right, and stress -remember what we said about stress, is it good or bad?
HANNAH: Neutral
DR. KIRKPATRICK: Very good. You’ve got your brain back. How about that she remembers. By the way, while we’re on that subject, let me tell you, you're probably going to find it a lot easier for you to focus now when you don't have so much pain. So learning is going to be a much easier task for you going forward.
That's right, stress is neutral. What the heck is neutral? What is that? Well stress is a biological response that you can't control, and you can make it either a negative or a positive experience. And one of the things we learned over the years is that there’s one thing that always predictably works in controlling stress and keeping it from being negative. What's that called, dad, what's that activity that we talked about putting stress under control
DAD: Physical activity
DR. KIRKPATRICK: There you go. Very good. Wow memory works well in the whole family here. Very good. By the way, he’s scored high - he’s got the highest score from me so far, okay. That's right, so water exercise and physical activity helps control the stress, therefore you're not going to get in the pool with a bunch of kids are you?
HANNAH: No
DR. KIRKPATRICK: Where the the kids are yelling and screaming and all that kind of stuff, okay
Now the next thing we talked about is medications. Now you're not on any strong medications, we call those narcotics, like Vicodin, Percocet and all that kind of stuff but we did say there is a role for those in treating RSD isn't there?
HANNAH: Yes
DR. KIRKPATRICK: If you get an acute injury, or for an example you go to the dentist and he starts doing a lot of things in your mouth, you can't handle the stress, like the pain from that, like other people can and it could set off the RSD, right?
HANNAH: Yes
DR. KIRKPATRICK: Now let's turn over to the parents here. Now you've been with her over the weekend. What do you think? Has her mood improved? Does she seem a little bit more hopeful than she was before the ketamine?
DAD: Yes sir, she has improved a lot. I mean her mood her attitude has changed a lot. Over the weekend she's been able to do activities that she hasn't been able to do in a year and a half, and we know, and we're optimistic, about it and know that she's just going to continue to get better with the physical treatment, physical exercise and still really looking forward to it. I'm so happy that she's doing good.
DR. KIRKPATRICK: Right. Now did you have any questions?
DAD: No sir
DR. KIRKPATRICK: Mom, do you have, would you kind of agree with all that?
MOM: Yes and she's really enjoying taking a bath now so the water doesn't feel like razor blades
DR. KIRKPATRICK: Right, right. I'm glad you brought that up because being able to take care yourself and hygiene and all that kind of stuff is really, really important okay. Even eating. Remember she had a lot of jaw pain, so she could enjoy eating now. She couldn’t do that before. Mom, do you have any questions?
MOM: No
DR. KIRKPATRICK: Okay now let's go back to Hannah. Hannah, do you have anything to add to what your mom and dad said about your experience? Okay. How about you, do you have any questions?
HANNAH: No
DR. KIRKPATRICK: I have a question for everybody here. Now we always try to learn from experiences and share that with others. Are all of you comfortable with us using this recording? Of course she's going to be back in about a month or two and I'm going to repeat all this. Are you comfortable with the idea of sharing this information with others out there so they can learn from your experience? Is that okay with you?
HANNAH: Yes
DR. KIRKPATRICK: Let’s make sure that's okay with your parents. Mom, Dad?
MOM: Yes
DAD: Yes absolutely.
DR. KIRKPATRICK: Okay, just wanted to make sure.
(Dr. Kirkpatrick returns to the conference in Havana)

DR. KIRKPATRICK: What I want to do now, I want to summarize for you what we call the take home message.
Okay, I wanted you to see the video. I wanted you to see the pain thresholds. I wanted to test both of you so you can appreciate the precision of the measurements of pain - reproducibility of the measurement so that you can see that the focus here is on objective measurement, so you as a doctor can feel confident that you're helping the patient and you’re not harming them especially when you're doing something new.
This ketamine treatment is new. The treatment is still being evolved in the United States. Now I have doctors coming to us, we are a nonprofit organization; they come to us to learn how to do this treatment properly.
If you don't do it properly, it will not succeed; but the most important thing I want you to get from this discussion today- informal, first acquaintance and so forth, is the idea of objective measurements and how important that is not just for you but for the patient as well.
|











 just how far you could open your mouth without causing any problems.
just how far you could open your mouth without causing any problems.