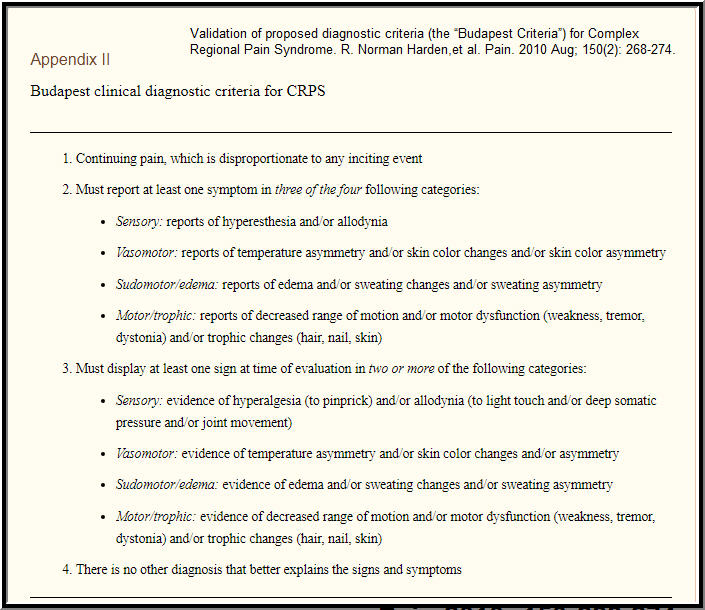
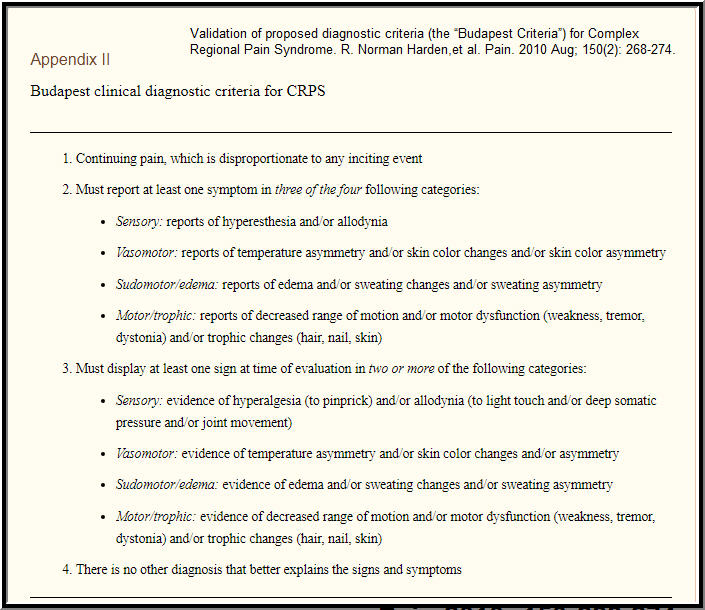
1-Continuing pain, which is disproportionate to any inciting event
Yes - Chronic pain in the upper right region of body documented at the Miami Children's Hospital Emergency Room for the first time four days after the bike accident. (November 8, 2014)
NOTE: The hospital record of 11/8/2014 establishes that the bike accident is causally related to the development of CRPS in the upper right extremity with subsequent spreading throughout the body. There is no evidence of problems in the upper right region of the patient's body prior to the bike accident. |
1-Continuing pain, which is disproportionate to any inciting event
Yes - Chronic pain in the upper right region of body documented at the Miami Children's Hospital Emergency Room for the first time four days after the bike accident. (November 8, 2014) |
2-Must report at least one symptom in three of the four following categories:
- Sensory: reports of hyperesthesia and/or allodynia
Yes- Allodynia (Page 2)
Yes-
Hyperesthesia - "Increased sensitivity to light and sound". (Page 1)
NOTE: Hyperesthesia is defined as an increase in the sensitivity of any of your senses, such as sight, sound, touch, and smell. It can affect just one or all of the senses.
- Vasomotor: reports of temperature asymmetry and/or skin color changes and/or skin color asymmetry
Yes- Asymmetrical warm sensations (Page 2)
Yes -Asymmetrical purple color changes (Page 2)
- Sudomotor/edema: reports of edema and/or sweating changes and/or sweating
Yes- Asymmetrical swelling (Page 2)
Yes- Asymmetrical sweating - Prior to sympathectomy (Page 2)
- Motor/trophic: reports of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
Yes- Decrease range of motion (Page 2)
Yes- Weakness (Page 2)
Yes- Dystonia(Page 2)
Yes- Asymmetrical brittle nails - right side (Page 2)
|
2-Must report at least one symptom in three of the four following categories:
- Sensory: reports of hyperesthesia and/or allodynia
Yes- Hyperesthesia - "Increased sensitivity to sound, light and touch, including clothing". (Pages 8, 9 and 10)
Yes- "Allodynia to pinprick." (Page 2)
- Vasomotor: reports of temperature asymmetry and/or skin color changes and/or skin color asymmetry.
Yes- Right hand turns blue. Page 8.
SEE NOTE BELOW
- Sudomotor/edema: reports of edema and/or sweating changes and/or sweating
SEE NOTE BELOW
- Motor/trophic: reports of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
Yes- "still experiencing weakness" in fingers. (Page 5)
Yes- Right hand stays in a "closed or clenched position" consistent with dystonia. (Pages 4 and 10)
NOTE:
Identifying abnormal function of the sympathetic nervous system is key to making the diagnosis of CRPS. In taking the clinical history of the patient, Dr. Rauck (Dr. R) failed to evaluate the patient for abnormal function of the sympathetic nervous system. Either through incompetence or with the intention to conceal the diagnosis of CRPS, Dr. R failed to objectively evaluate the patient for CRPS.
The patient had a sympathetically performed which would create abnormal function of the sympathetic nervous system. Dr. R failed to question the patient for abnormal function of the sympathetic nervous system before the sympathectomy had been performed
For example:
In the video, he never questioned the patient about asymmetrical changes in temperature in the affected regions of the patient's body before the sympathectomy.
In the video, he never question the patient about asymmetrical changes and sweating or swelling or sweating before the sympathectomy.
Even when he questioned the patient about asymmetrical changes in color in her upper extremities, he minimized in his report the significance of this characteristic finding with CRPS.
For example, in his report he wrote, "She states that there are only been an occasional time that her fingers in the right hand would turn blue." However, in the video, the patient stated, "The fingers turn blue mainly in the right hand." |
3-Must display at least one sign at time of evaluation in two or more of the following categories:
- Sensory: evidence of hyperalgesia (to pinprick) and/or allodynia (to light touch and/or deep somatic pressure and/or joint movement)
YES- Asymmetrical allodynia (Page 3)
NOTE: Demonstrated objectively using quantitative sensory testing.
- Vasomotor: evidence of temperature asymmetry and/or skin color changes and/or asymmetry
NO
- Sudomotor/edema: evidence of edema and/or sweating changes and/or sweating asymmetry
NO
- Motor/trophic: evidence of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
YES-Asymmetrical decrease range of motion (Page 2)
YES-Asymmetrical weakness (Page 2)
YES- Dystonia (Page 2)
YES-Asymmetrical atrophy (Page 2)
|
3-Must display at least one sign at time of evaluation in two or more of the following categories:
- Sensory: evidence of hyperalgesia (to pinprick) and/or allodynia (to light touch and/or deep somatic pressure and/or joint movement)
YES- Asymmetrical allodynia (Page 10)
YES- Tenderness in upper chest in a widespread distribution. (Page 10)
- Vasomotor: evidence of temperature asymmetry and/or skin color changes and/or asymmetry
SEE NOTES BELOW ABOUT THE IME VIDEO: CLICK HERE
- Sudomotor/edema: evidence of edema and/or sweating changes and/or sweating asymmetry
SEE NOTES BELOW ABOUT THE IME VIDEO: CLICK HERE
- Motor/trophic: evidence of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nail, skin)
YES- Deceased range of motion of right hand. Right hand went into a curled position when splint was removed which is consistent with dystonia. (Page 11) In the video, the patient obviously had severe bilateral dytonia of the upper extremities with the right side being worse than the left. Yet the word "dystonia" is not reported as a finding either as a symptom or sign of CRPS. Dystonia is a characteristic finding in patients with CRPS.
On March 16, 2016, Dr. Andrew Sherman, diagnosed "dystonia" in the patient.
|
4-There is no other diagnosis that better explains the signs and symptoms
YES- CRPS best explains the signs and symptoms |
4-There is no other diagnosis that better explains the signs and symptoms
YES- CRPS best explains the signs and symptoms |